Back to 2024 Abstracts
OVERALL SURVIVAL OF PATIENTS WITH CLINICAL COMPLETE RESPONSE AFTER RADIOCHEMOTHERAPY FOR ESOPHAGEAL CANCER: SHOULD A WATCHFUL WAITING STRATEGY BE THE NEW STANDARD OF CARE?
Sarah Gerber
*, Hossein Hemmatazad, Martin D. Berger, Dino Kröll, Reiner Wiest, Tobias Haltmeier, Yves Borbély
Universitat Bern Medizinische Fakultat, Bern, Bern, Switzerland
Background
The current standard of care for the treatment of esophageal cancer (EC) in a curative intent consists of neoadjuvant radiochemotherapy (RCT) followed by resection. However, an organ-sparing approach with a watchful waiting (WW) strategy and resection only in case of cancer recurrence is gaining importance in patients with clinical complete response (cCR) after RCT. Nevertheless, data on overall survival, particularly in subgroups with and without tumor recurrence, is limited. We aim to compare the overall survival (OS) rates in patients with cCR based on their initial management and at time of recurrence.
Methods
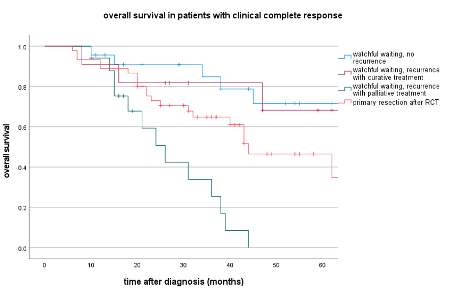
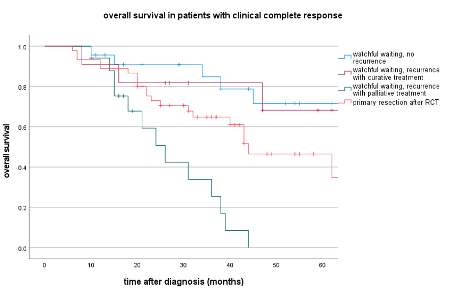
We retrospectively analyzed data from all potentially curable EC patients with cCR to RCT between January 2014 and December 2021 at a tertiary university hospital. Clinical complete response was defined as no evidence of vital cancer cells in biopsy of restaging endoscopy. Patient data were extracted from prospectively recorded electronic medical files. OS- and disease-free survival was calculated using Kaplan-Meier survival analysis. Four groups were compared: resection after RCT, WW without recurrence, WW with recurrence treated in curative, and WW with recurrence treated in palliative intent.
Results
Of 96 patients with cCR after RCT, 45 underwent resection (47%), and 51 (53%) were followed up in a WW approach. There were no significant differences in baseline patient or tumor characteristics.
In the WW group, 28 patients (55%) had cancer recurrence. Of those, 11 patients (39%) underwent either salvage esophagectomy or endoscopic submucosal dissection with curative intent.
Mean OS was 47.1 months (min 39.2 – max 55.1) in patients with initial resection after RCT, 71.7 months (59.4 – 84.1) in patients with WW and no recurrence, 55.6 months (42.3 – 69.0) in patients with recurrence treated in curative and 26.6 months (20.9 – 32.4) in palliative intention.
There was no significant difference in OS between patients with WW and either no recurrence and WW with recurrence treated in curative intention (p=0.716). However, OS was significantly longer in those two patient groups than in patients with primary resection (p=0.031) and WW patients with recurrence and palliative treatment (p<0.001), (Table 1).
Conclusion
In a WW concept after RCT for EC, patients with cancer recurrence can achieve the same OS as patients without recurrence if treated with curative intention. Moreover, OS in both those patient groups was superior to that of patients undergoing direct resection after RCT, supporting the WW approach as at least safe and applicable in clinical practice. Further prospective data are needed to determine the value of WW as standard of care for patients with cCR following neoadjuvant RCT.
Back to 2024 Abstracts