Back to 2024 Abstracts
DELTA-IRP AS A NEW HIGH-RESOLUTION MANOMETRY METRIC TO PREDICT THE POSITIVE OUTCOME OF LAPAROSCOPIC HELLER-DOR IN PATIENTS WITH ACHALASIA
Andrea Costantini
*, Matteo Pittacolo, Giulia Nezi, Luca Provenzano, Giovanni Capovilla, Loredana Nicoletti, Francesca Forattini, Arianna Vittori, Lucia Moletta, Matteo Santangelo, Michele Valmasoni, Edoardo V. Savarino, Renato Salvador
Azienda Ospedale Universita Padova, Padova, Veneto, Italy
IntroductionThere is no consensus on the definition of failure after treatment in patients with esophageal achalasia. Indeed, the Eckardt score (ES) is commonly used to define clinical outcome, but objective metrics based on high-resolution manometry (HRM) or other diagnostic methods are lacking. Aim of this study was to identify at HRM an objective parameter useful to predict a positive outcome after surgical treatment with laparoscopic Heller-Dor (LHD).
MethodsPatients who had undergone LHD between 2012 and 2022, with pre- and postoperative HRM at our Center, were consecutively enrolled. Exclusion criteria were radiological stage IV, previous endoscopic or surgical myotomy, pre- or postoperative conventional manometry. Patients were divided according to the outcome of treatment between success group (SG), in case of symptom relief or resolution, and failure group (FG) in case of an ES>3 or the need for additional treatment. Patients were evaluated with ES, barium swallow, endoscopy and HRM before and after surgery. Further to the traditional HRM metrics commonly evaluated, we also measured the difference between median values of pre- and postoperative IRP (Delta-IRP). A ROC curve analysis was applied to assess the accuracy of each HRM parameter identified.
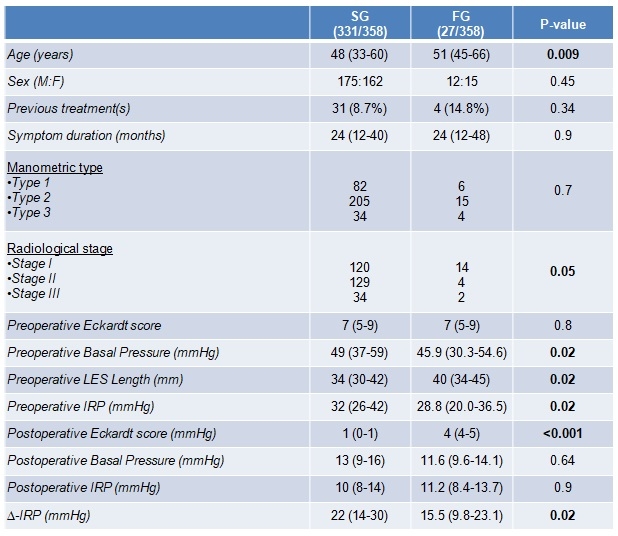
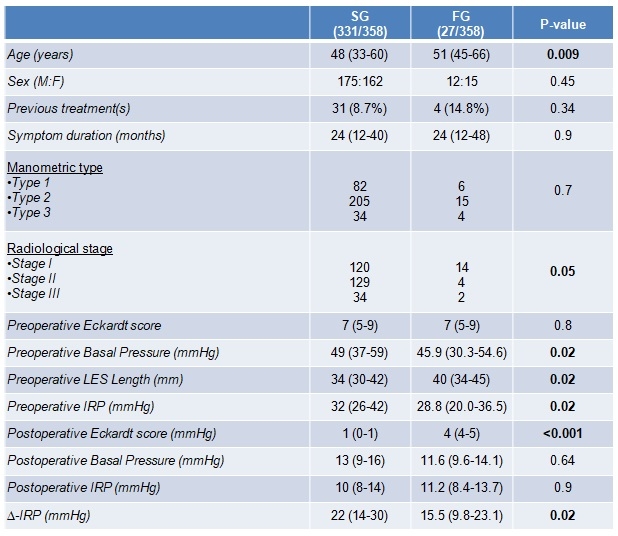
ResultsIn the study period, 358 patients (F:M=177:187) were recruited [median age: 49 years (IQR:36-60)], with 331 patients in the SG and 27 patients in the FG (Table 1). The surgical procedures were completed laparoscopically in all patients; there were 9 mucosal lesions all in the SG. No statistically significant difference was found in the preoperative manometric type, the symptom duration and the history of previous treatments, whereas the preoperative IRP was higher in SG [33 mmHg (IQR:26-43)] than in FG [27.4 mmHg (IQR:20.3-32.7), p<0.001]. The postoperative IRP was similar between the two groups [10 mmHg (IQR:8-14) vs 12.4 mmHg (IQR:8.7-13.9), p=0.5]. However, the Delta-IRP was higher in the SG [22 mmHg (IQR:15-31)] than in the FG [14.3 mmHg (IQR:9.9-18.3), p=0.04].
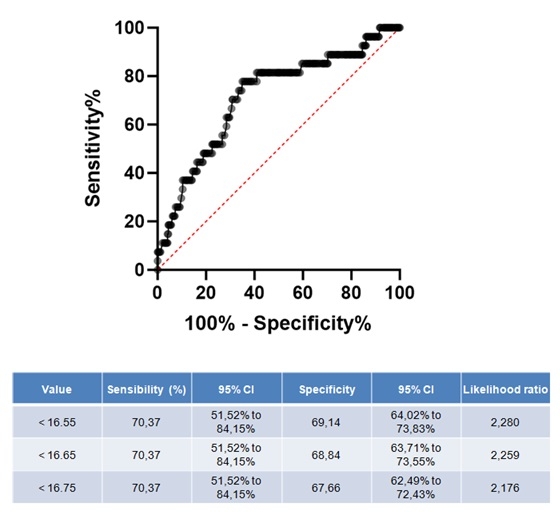
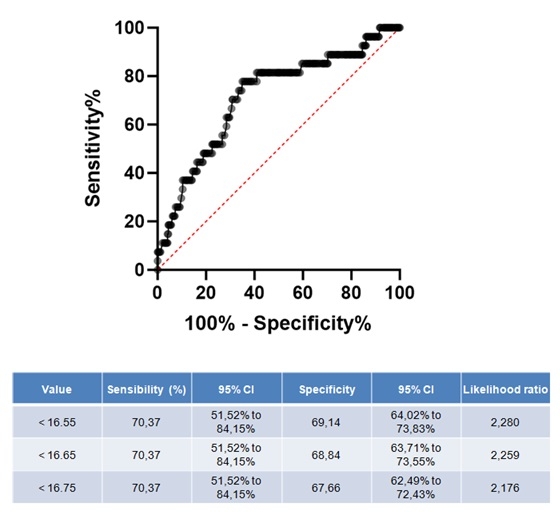
At univariable analysis, age (p<0.01), preoperative IRP (p<0.01), Delta-IRP (p<0.001), radiological stage (p<0.01), and LES total length (p=0.045) were the factors able to predict a positive clinical outcome. At multivariable analysis, the Delta-IRP was the only parameter independently related to clinical success (p<0.01, OR:0.94, CI 5%-95%:0.89-0.99). The ROC curve for the Delta-IRP showed an area under the curve that was equal to 0.71, with a threshold value set at 16.55 mmHg (sensibility 71%, specificity 70%) (Figure 1).
ConclusionsOur data showed that the Delta-IRP with a threshold of 16.5 mmHg could represent a new objective tool to predict the positive outcome of LHD in patients with esophageal achalasia.
Back to 2024 Abstracts