Back to 2024 Abstracts
DOES TIMING OF ILEOSTOMY CLOSURE IMPACT POSTOPERATIVE MORBIDITY?
Maxwell D. Mirande
*1, Katherine Bews
1, Justin T. Brady
2, Dorin Colibaseanu
3, Sherief Shawki
1, William Perry
1, Kevin T. Behm
1, Kellie L. Mathis
1, Nicholas P. McKenna
11Surgery, Mayo Clinic Minnesota, Rochester, MN; 2Mayo Clinic Arizona, Scottsdale, AZ; 3Mayo Clinic in Florida, Jacksonville, FL
Background: A diverting loop ileostomy (DLI) is commonly constructed for protection of high-risk anastomoses to reduce the morbidity of an anastomotic leak. Closure typically occurs at 12 weeks after formation. The idea of earlier closure has been raised in attempts to reduce the morbidity associated with DLIs. Therefore, we aimed to determine whether time to stoma reversal impacts postoperative morbidity after DLI closure.
Methods: A retrospective review was conducted using the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database for adult patients who underwent a DLI closure between January 2012 and December 2021 across three sites of a multistate health system. Time to DLI closure was stratified into three groups: ≤ 12 weeks (early), 12.01-24 weeks (standard), or 24.01-36 weeks (delayed). To avoid introducing bias from patients with prolonged diversion, patients who had their DLI > 36 weeks after formation were excluded. Additional data points of interest were obtained from the electronic medical record (EMR). The primary outcome was major morbidity after DLI closure, which included organ space infection, return to the operating room, and readmission, amongst other complications. For patients with an organ space infection, the EMR was reviewed to determine whether it was related to the small bowel anastomosis or from the protected anastomosis. Univariate comparisons were performed between the time to DLI closure groups. Potential risk factors for major morbidity after DLI closure were assessed by univariate comparisons followed by multivariable logistic regression.
Results: A total of 482 patients underwent DLI closure (Institution A,
n=331 [69%], Institution B,
n=77 [16%], and Institution C,
n=74 [15%]). Eighty-four patients underwent early closure (17%), 300 underwent standard closure (62%), and 98 had delayed closure (20%). The most common diagnosis at DLI formation was cancer (
n=211, 44%), followed by ulcerative colitis (
n=144, 30%) and diverticular disease (
n=81, 17%). Patients in the early closure group more commonly had ulcerative colitis or diverticular disease and had a lower ASA physical status than patients with delayed closure (both
p<0.05).
There were no significant differences in overall major morbidity or in its individual components amongst the time to DLI closure groups. There was no difference in anastomotic leak rates from the protected anastomosis (Early,
n=1 [1%], Standard,
n=2 [1%], and Delayed,
n=0 [0%];
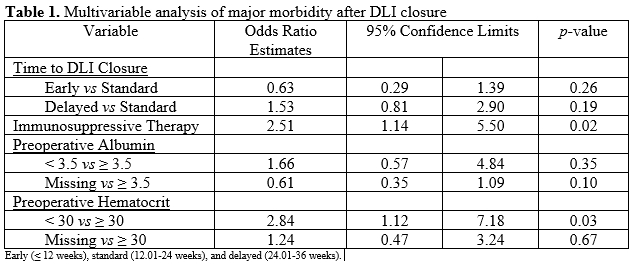
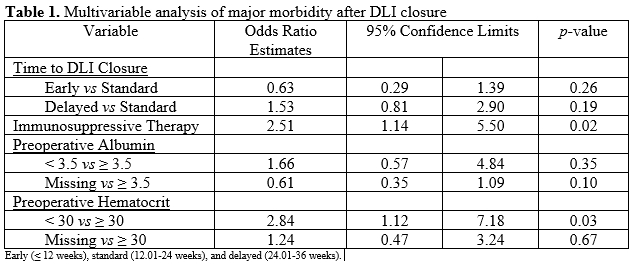
p=0.5). On multivariable analysis, immunosuppressive therapy and preoperative hematocrit < 30% were significant risk factors for major morbidity after DLI closure. Time to DLI closure was not a significant risk factor (Table 1).
Conclusion: Major morbidity did not differ by time to DLI closure group indicating that closure before 12 weeks may be safe in select patients.
Back to 2024 Abstracts