Back to 2024 Abstracts
HEALING OF PERINEAL WOUNDS AFTER PROCTECTOMY FOR CROHN'S DISEASE: A SYSTEMATIC REVIEW AND META-ANALYSIS
Ali Alipouriani
*, Kamil Erozkan, Lukas Schabl, Stefan D. Holubar
Colorectal Surgery, Cleveland Clinic, Cleveland, OH
Background: Non-healing perineal wounds are common in patients undergoing proctectomy for Crohn's disease. We systematically reviewed the literature and performed a meta-analysis to estimate the pooled proportion of perineal wound healing after proctectomy for Crohn's disease.
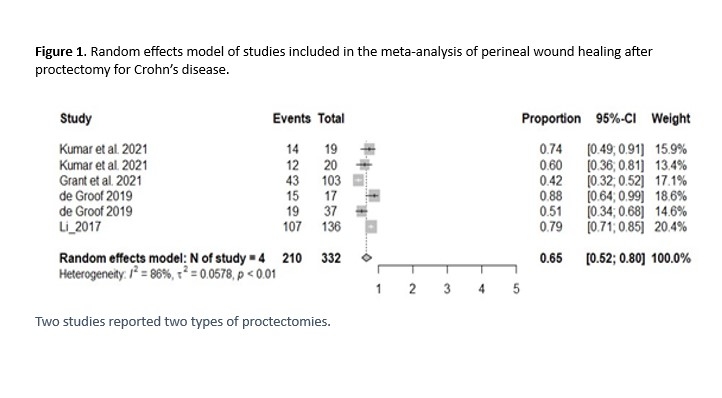
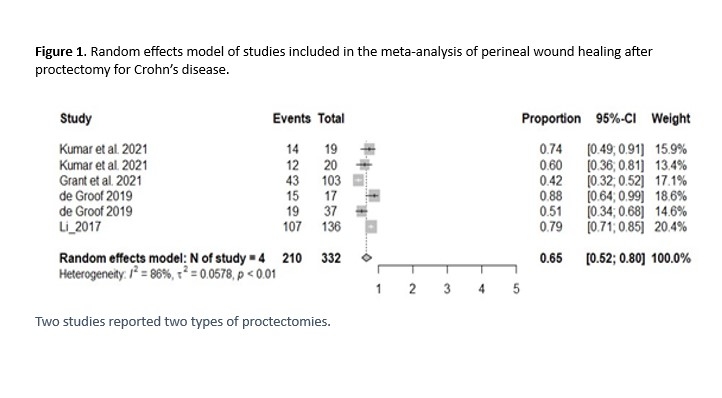
Methods: A comprehensive literature search was conducted in PubMed, Embase, and Scopus databases to identify relevant studies reporting perineal wound healing after proctectomy in patients with Crohn's disease from 2010 to 2023. Articles were screened and those reporting perineal wound healing rates after proctectomy were included. Data on the study characteristics and proportion of healed wounds were extracted. Random effects meta-analysis was performed to estimate the pooled proportion and 95% confidence intervals using the ‘meta' package in R. Heterogeneity was assessed using the I
2 statistic.
Results: The literature search yielded 501 articles, of which 252 articles remained after removing duplicates. After screening the titles and abstracts, four retrospective cohort studies involving 332 patients with Crohn's who underwent proctectomy were included in the meta-analysis. Across the four studies, the pooled proportion of completely healed perineal wounds at 6 months was 65% (95% CI 52%-80%) and at 12 months was 70% (95% CI 60%-83%). Significant heterogeneity was found between studies (I
2=86% at 6 months). Only one study examined the predictors of impaired healing after proctectomy. Factors such as age, sex, BMI, smoking, steroid use, presence of high fistula-in-ano, and surgical technique were not significantly associated with impaired healing in univariate and multivariate analyses in this study. However, preoperative perineal sepsis was independently associated with impaired healing in the univariate and multivariate analyses in this study (p = 0.001). Study 4 included both Crohn's disease (n=54) and ulcerative colitis (n=20) patients who underwent proctectomy and reported fewer overall perineal complications in patients with UC than in those with Crohn's disease (15% vs. 46.3%, p=0.01).
Conclusions: This meta-analysis revealed complete perineal healing in 70% of patients with Crohn's 12 months after proctectomy. Significant heterogeneity was observed between the studies. This review highlights the gaps in the best practices for optimizing perineal wound healing after proctectomy. These findings suggest the need to study techniques, such as vacuum-assisted closure and flap reconstruction. Further research is needed to identify modifiable factors to increase healing rates and develop evidence-based protocols for surgical approach, wound closure, and postoperative care in Crohn's disease patients.
Back to 2024 Abstracts