Back to 2024 Abstracts
A REVIEW OF MIDGUT MALROTATION IN THE ADULT POPULATION: DIAGNOSIS, TECHNIQUES AND OTCOMES OF THE LAPAROSCOPIC LADD'S PROCEDURE.
Ibrahim A. Gomaa
*1, Maxwell D. Mirande
2, Sarah Armenia
2, Eric Dozois
1, William Perry
11Mayo Clinic Division of Colon and Rectal Surgery, Rochester, MN; 2Mayo Clinic Department of Surgery, Rochester, MN
IntroductionIntestinal malrotation results from abnormal embryonic midgut rotation that results in positioning of the small bowel on the right and the colon on the left. Further, Ladd's bands commonly fix the duodenum and cecum to the abdominal wall. Adults may be asymptomatic or present with acute obstruction or abdominal pain. A Ladd's procedure is the treatment of choice, however long-term outcomes of a laparoscopic Ladd's procedure are not well-documented. This study aims to review the presentation, management, and outcomes in adults who underwent a laparoscopic Ladd's procedure at a single institution.
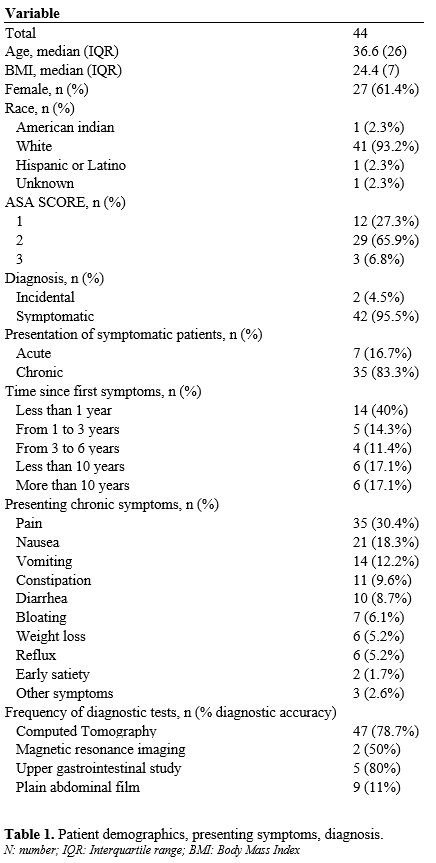
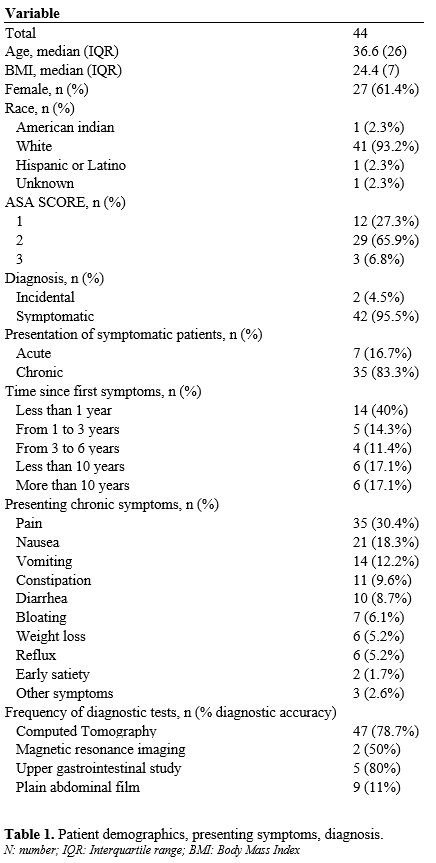
Methods A retrospective review of health records was undertaken at Mayo Clinic, Rochester to identify adult patients with malrotation who had a laparoscopic Ladd's procedure between January 1, 1995, and June 1, 2022. Patient demographics, presentation, operative details, outcomes, and follow-up were recorded. Patients were then invited to partake in a structured phone interview to assess symptoms and resolution, quality of life, and likelihood of recommending the procedure to a friend or family with the same condition. This multi-methods analysis was approved by the Institutional Review Board.
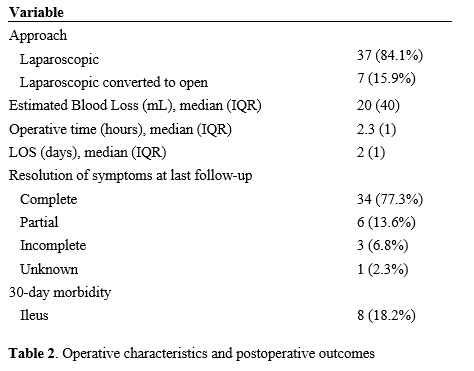
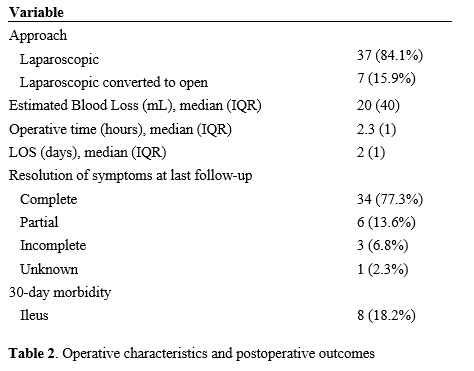
ResultsA total of 44 patients underwent Laparoscopic Ladd's procedure: median age was 36.6 (23); 27 (61.4%) were females; median BMI was 24.4 (7); and 41 (93%) were classified as ASA I or II. Forty-two (95.5%) were symptomatic, with 7 (16.7%) presenting acutely. Although abdominal CT was the most frequently utilized imaging modality, diagnostic accuracy was 78.7% compared with an upper gastrointestinal contrast study that was 80% accurate. Seven (15.9%) laparoscocpic procedures converted to open to ensure safe dissection. The median estimated blood loss was 20mL, operative time was 2.3 hours, and hospital stay was 2 days. Eight (18%) had post-operative ileus, with no other documented 30-day morbidity. Median follow-up was 7 years with 33 (75%) experiencing complete resolution of symptoms and 7 (15.9%) experiencing partial resolution.
Twenty-eight participants (63.6%) completed the phone interviews. When asked to compare their current symptoms to those pre-operatively, 22 (78.6%) noted that they were significantly better. Further, 24 (85.7%) reported that their quality of life was significantly better after surgery. Finally, a majority (27, 96.4%) would recommend the procedure to a friend or family member with the same condition.
ConclusionLaparoscopic Ladd's procedure is a safe and effective operation with good post-operative outcomes. Of note, it has a positive impact on quality-of-life post-surgery.
Back to 2024 Abstracts