Back to 2024 Abstracts
ROBOTIC PARA-AORTIC LYMPH NODE DISSECTION FOR COLORECTAL CANCER: SHORT-TERM OUTCOMES
Atsushi Ikeda
*, Kentaro Ochiai, Neal Bhutiani, Michael White, Oliver Peacock, Abhineet Uppal, Craig A. Messick, Brian K. Bednarski, Y. Nancy You, John M. Skibber, George J. Chang, Tsuyoshi Konishi
Surgical Oncology, MD Anderson Cancer Center, Houston, TX
Background: Although paraaortic lymph node (PALN) metastasis of colorectal cancer is beyond regional disease, previous studies suggested surgical dissection of PALN may serve as a curative therapeutic approach in patients with limited disease burden. However, the procedure is frequently associated with intraoperative bleeding and postoperative complications. We hypothesize that a robotic approach may contribute to reducing bleeding and complications. This study aims to investigate the safety and feasibility of robotic PALN dissection for colorectal cancer.
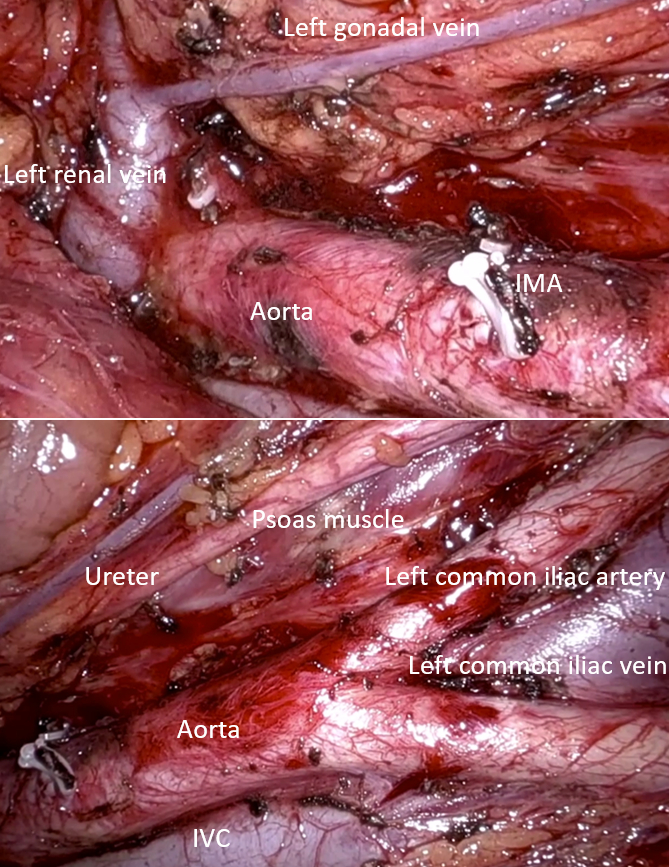
Methods: This is a single-center retrospective study performed in an NCI-designated comprehensive cancer center. The institutional prospectively maintained database was queried for colorectal cancer patients who underwent radical PALN dissections using a robotic approach for radiologically suspected PALN metastasis between 2011 and 2023. This study included radical systematic PALN dissection of the region defined by left renal vein, aortic bifurcation, right side edge of the aorta, and left gonadal vein (Figure). Sampling or limited lymphadenectomy of PALNs were excluded from the study.
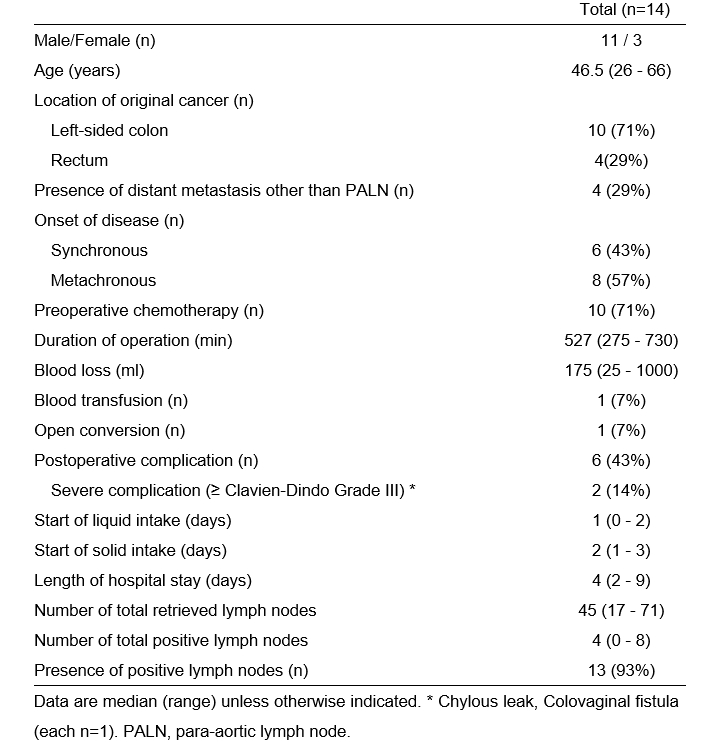
Results: Among 154 patients who underwent PALN dissection during the study period, 32 underwent robotic surgery, and 14 were eligible for the study after excluding sampling or limited lymphadenectomy. The location of the primary tumor was the left colon in 10 (71%) patients and the rectum in 4 (29%) patients (Table). The timing of PALN metastasis was synchronous in 6 (43%) patients and metachronous in 8 (57%) patients. Twelve patients underwent simultaneous colorectal resection. Preoperative chemotherapy was given to 10 (71%) patients. One (7%) patient needed open conversion due to intraoperative bleeding. Median operative time was 527 minutes (range, 363 – 608 minutes), and median blood loss was 175 mL (range, 105 - 250 mL). one patient required intraoperative blood transfusion. Overall postoperative complications occurred in 6 (43%) patients including 2 (14%) complications ≥ grade III: grade IIIb colovaginal fistula and grade IIIa chylous leak (each n = 1). No patients developed urinary dysfunction. The median hospital stay was 3 days. The median number of retrieved lymph nodes was 45 (range, 17 - 71). Pathologically positive lymph nodes were present in 13 (93%) patients.
Conclusion: Although the study is limited by a single institutional study performed by experienced robotic surgeons in a high-volume cancer center, initial experiences of robotic PALN dissection demonstrated safe and feasible short-term outcomes with acceptable rates of severe postoperative complications and high lymph node yield. Robotic surgery is a feasible surgical approach for colorectal cancer patients with positive PALN.
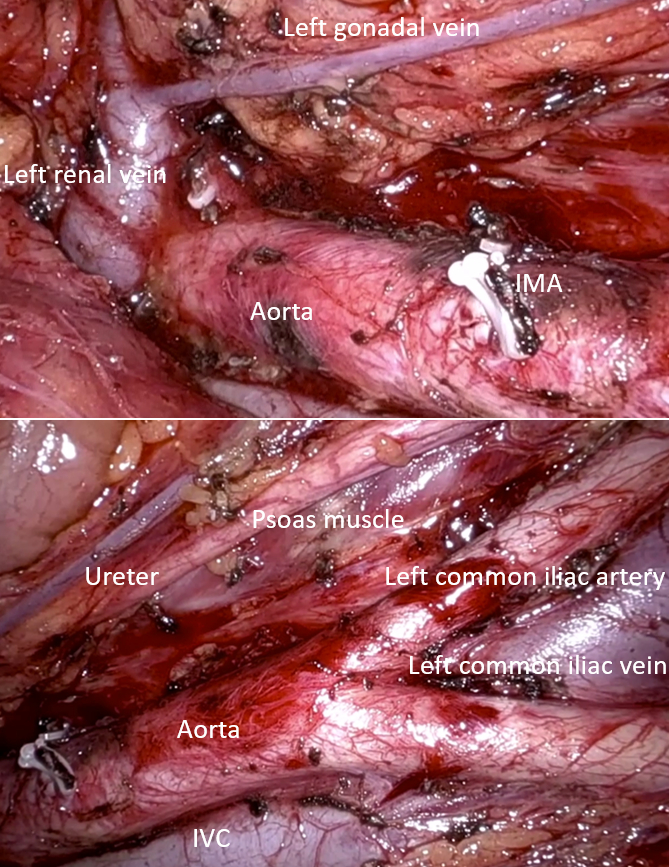
Figure
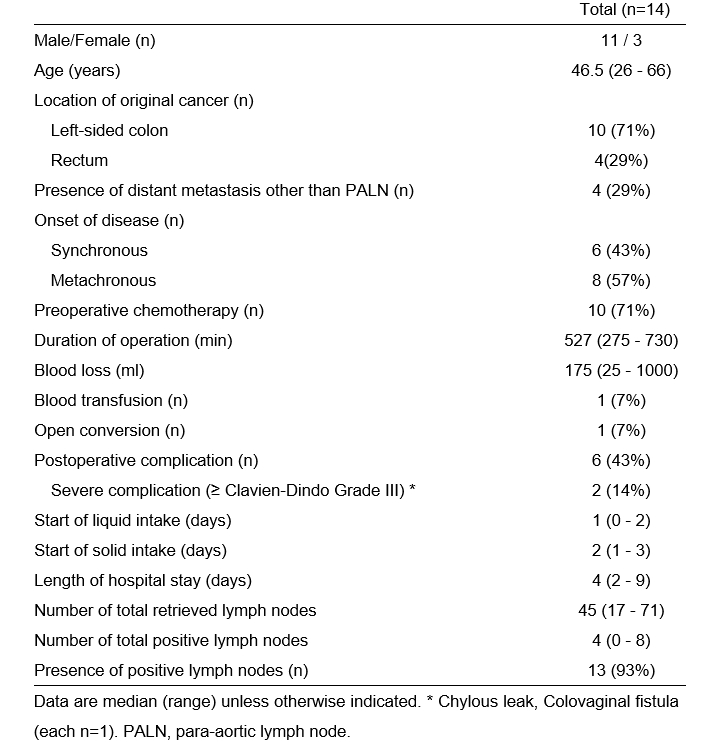
Table
Back to 2024 Abstracts