Back to 2024 Abstracts
MALE GENITOURINARY DYSFUNCTION AFTER PRIMARY AND REOPERATIVE ILEONAL POUCH SURGERY
Oscar Hernandez Dominguez
*, Christopher Prien, Raha Almarzooqi, Imran Khan, Mikhael Belkovsky, Himani Sancheti, Nicole E. Brooks, Olga Lavryk, Arielle E. Kanters, Jeremy M. Lipman, David Liska, Michael Valente, Emre Gorgun, Tracy L. Hull, Scott Steele, Stefan D. Holubar
Colorectal Surgery, Cleveland Clinic, Cleveland, OH
BackgroundRestorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the preferred surgical treatment for patients with IBD or FAP. As these diseases often manifest during adolescence or early adulthood, treatment effects on genitourinary function (GU) and sexual function are of paramount importance. However, the reoperative IPAA (R-IPAA) effects on male GU function and sexual function compared to primary IPAA (P-IPAA) are not known. Therefore, we conducted a survey study to compare the long-term GU functionality of P-IPAA and R-IPAA long-term GU functionality male patients. We hypothesized that R-IPAA is associated with higher GU-dysfunction compared to R-IPAA.
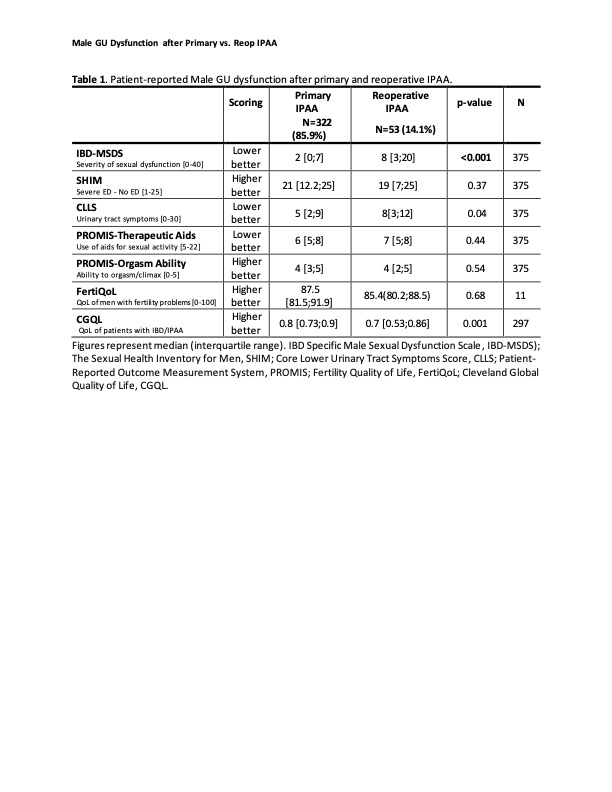
MethodsAll adult male patients who underwent IPAA at a single tertiary hospital between 1983 and 2023 were identified, and demographics and clinical data were obtained from our prospectively maintained pouch registry. Patients were surveyed using validated GU function, sexual function, fertility, and quality of life questionnaires (
Table 1). The primary outcome was the composite survey scores. Patients were stratified into P-IPAA or R-IPAA groups; R-IPAA was defined as IPAA reconstruction, revision, or excisions. Patients post prostatectomy were excluded.
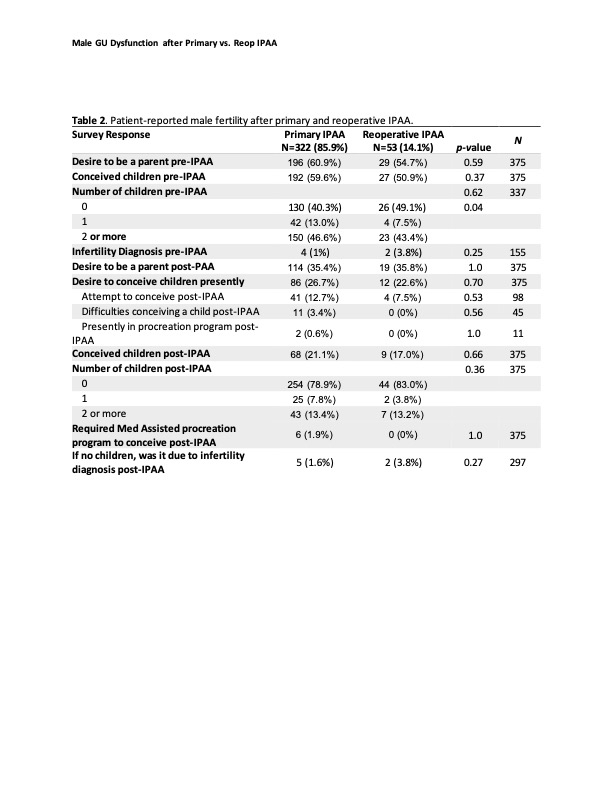
ResultsA total of 1,902 patients were surveyed, and 504 (26.5%) submitted a response. After the exclusion criteria, 375 responses were analyzed: 322 (85.9%) P-IPAA and 53 (14.1%) R-IPAA, which included 30 redo IPAA, 12 revisions, and 11 excisions. In both groups, most patients had ulcerative colitis (89.4 vs. 86.8%). P-IPAA compared to R-IPAA had a similar age at surgery (40.7 vs. 41.4, p=0.64), similar age at survey (55.7 vs. 56.0, p=0.97), and a similar year interval between surgery and survey (15.0 vs. 14.6, p=0.62). The P-IPAA group had less severe sexual dysfunction (IBD-MSDS, 2.0 vs. 8.0, p<0.001) and fewer urinary tract symptoms (CLLS, 5 vs. 8, p=0.04) than the R-IPAA group. No significant difference was observed between P-IPAA and R-IPAA in erectile dysfunction (SHIM score 21 vs. 19, p=0.37), use of therapeutic aids for sexual activity (6 vs. 7, p=0.44), or orgasm ability (4 vs. 4, p=0.54). There were no differences in infertility (5 vs. 2, p=0.27), or infertility impact on quality of life between the P-IPAA and R-IPAA groups (FertiQoL, 87.5 vs. 85.4, p=0.68) (
Table 2). Male P-IPAA had a higher overall quality of life (CGQoL, 0.8 vs. 0.7, p=0.001).
ConclusionPrimary-IPAA was associated with increased sexual function, urinary control, and overall higher global quality of life compared to R-IPAA. Although reoperating in the pelvis to address failing IPAA may raise concerns for nerve disruption and postoperative GU pathology, patients may be counseled that orgasm ability and fertility do not worsen.
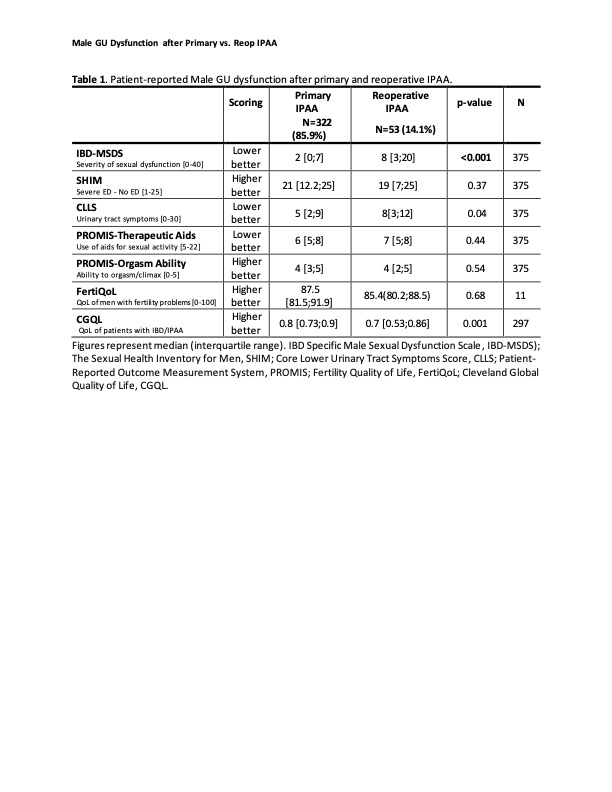 Table 1
Table 1. Patient-reported Male GU dysfunction after primary and reoperative IPAA.
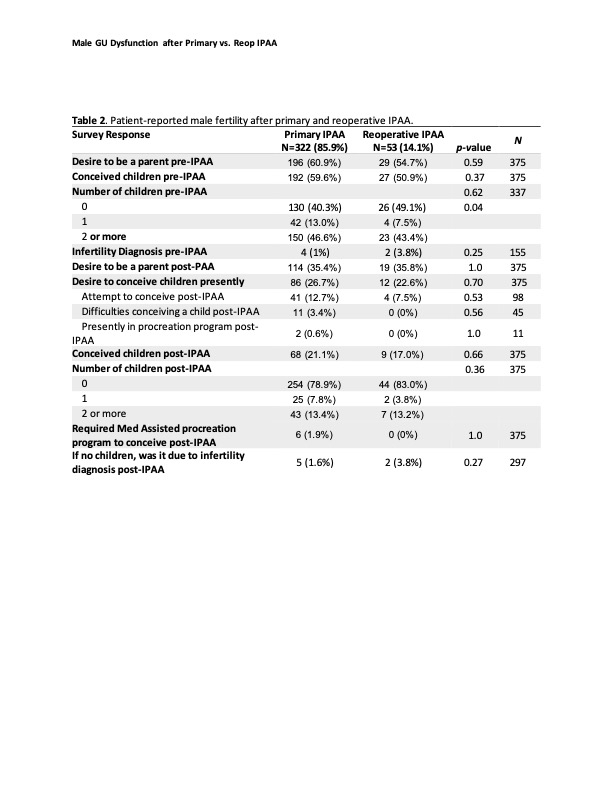 Table 2
Table 2. Patient-reported male fertility after primary and reoperative IPAA
Back to 2024 Abstracts