Back to 2024 Abstracts
MALE GENITOURINARY DYSFUNCTION AFTER MINIMALLY INVASIVE AND OPEN ILEOANAL POUCH
Oscar Hernandez Dominguez
*, Christopher Prien, Raha Almarzooqi, Mikhael Belkovsky, Imran Khan, Himani Sancheti, Nicole E. Brooks, Olga Lavryk, Arielle E. Kanters, Jeremy M. Lipman, David Liska, Emre Gorgun, Michael Valente, Tracy L. Hull, Scott Steele, Stefan D. Holubar
Colorectal Surgery, Cleveland Clinic, Cleveland, OH
Background Restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the preferred surgical treatment for IBD or FAP. As these diseases often manifest during adolescence or early adulthood, treatment effects on genitourinary function (GU), sexual function, and fertility are clinically important. However, the difference in male GU function and fertility between minimally invasive IPAA (MIS-IPAA) and open IPAA is unclear. We conducted a patient-reported survey study to compare long-term GU functionality in male patients after MIS-IPAA versus open-IPAA.
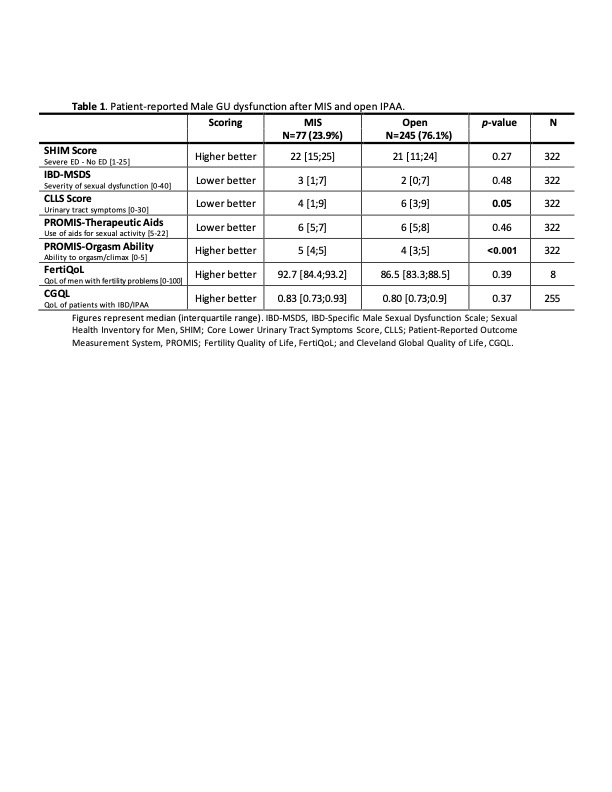
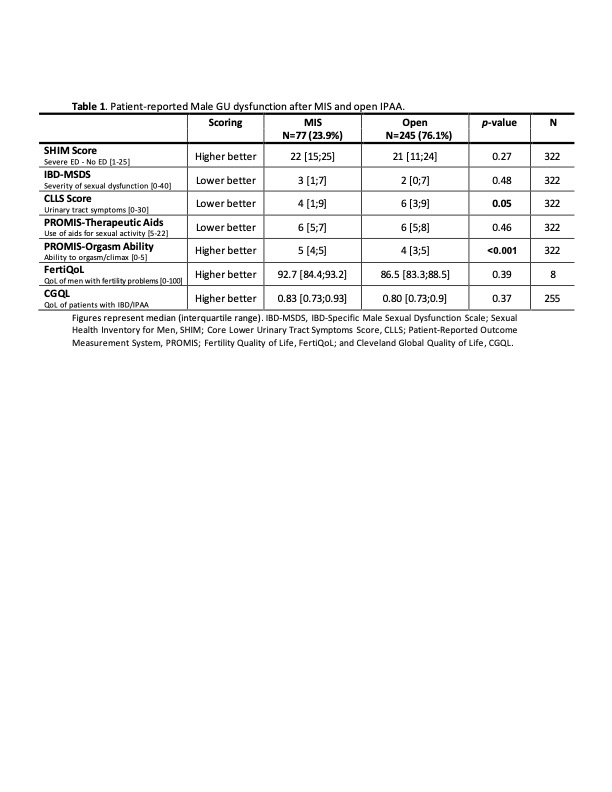
Methods All adult male patients who underwent IPAA at a single quaternary hospital between 1983 and 2023 were identified, and demographics and clinical data were obtained from our prospectively maintained pouch registry. Male patients were surveyed using validated GU function, sexual function, fertility, and quality of life questionnaires (Table 1). The primary outcome was the composite survey scores. Patients were stratified into MIS-IPAA (laparoscopic, robotic, single-incision surgery) or open-IPAA groups based on the mode of pelvic/rectal dissection. Reoperative IPAA procedures (revisions, redo, and excisions), incomplete surveys, patients with permanent ileostomy, or post-prostatectomy proctectomy status were excluded.
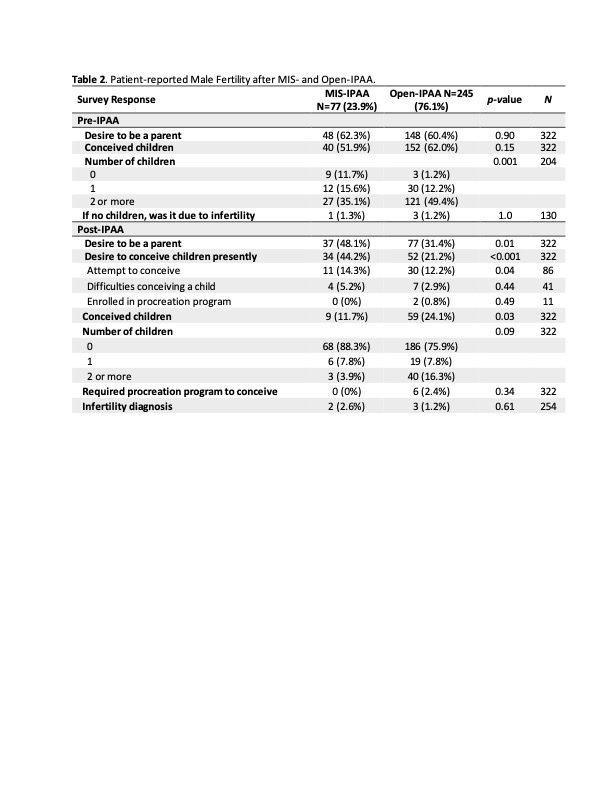
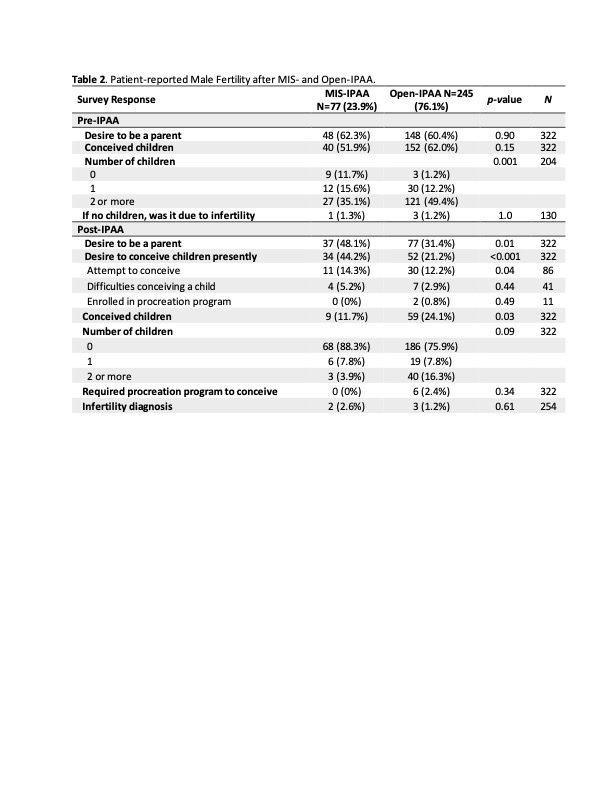
Results A total of 1,902 patients were surveyed and 504 (26.5%) responded. After exclusion criteria, 322 responses were analyzed: 245 (76.1%) open-IPAA and 77 (23.9%) MIS-IPAA. In both groups, most patients had ulcerative colitis (89 vs. 89%). Compared to open-IPAA, MIS-IPAA had a similar age at surgery (39.6 vs. 41.0, p=0.41), younger age at survey (47.0 vs 58.4, p<0.001), and shorter interval between surgery and survey (7.4 vs. 17.4, p<0.001). More MIS-IPAA patients achieved orgasm than those with open-IPAA (5 vs. 4, p=0.001) and had fewer lower urinary tract symptoms (LUTS) (CLLS, 4 vs. 6, p=0.037). No significant difference was observed between MIS and open IPAA in erectile function (SHIM score 22 vs. 21, p=0.27), male sexual dysfunction (IBD-MSDS, 3 vs. 2, p=0.48), or use of therapeutic aids for sexual activity (6 vs. 6, p=0.46). There were no differences in difficulty conceiving a child (4 vs. 7, p=0.44), infertility (2 vs. 3, p=0.61), or infertility impact on quality of life between the MIS and open-IPAA groups (FertiQoL, 92.7 vs 86.5, p=0.39) (Table 2). There was no difference in overall global quality of life (CGQoL, 0.83 vs 0.80, p=0.37).
Conclusion Men who underwent minimally invasive IPAA had higher preservation of orgasm ability and fewer lower urinary symptoms than open IPAA. There was no difference in erectile function, need for therapeutic aids for sexual function, or fertility between MIS and the open approach to pelvic dissection in IPAA. MIS approaches to IPAA appear to be associated with a lower rate of male pelvic nerve dysfunction than open IPAA.
Back to 2024 Abstracts