Back to 2024 Abstracts
A CROSS SECTIONAL ANALYSIS OF ANXIETY AND DEPRESSION AMONG COLON CANCER PATIENTS
Russell J. Hollis
*1, Abdullah Khalid
1, Elizabeth Nilsson Sjolander
1, Maria Cardenas Sanchez
1, Rachel N. Harvey
1, Manav J. Shah
2, Andrea Zimmern
11Surgery, Northwell Health, New Hyde Park, NY; 2Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY
Introduction:
Colon cancer (CCA) is one of the most common cancers in the United States. While survivorship for CCA has improved, there are challenges pertaining to mental health. Studies suggest that 13-57% of patients with CCA experience depression, and 5.7-20.9% experience anxiety. The General Anxiety Disorder-7 (GAD-7) and Patient Health Questionnaire-8 (PHQ-8) are validated diagnostic tools used to diagnose GAD and major depressive disorder (MDD), respectively. We aim to identify clinical and biopsychosocial factors associated with GAD and MDD in patients diagnosed with CCA.
Methods:
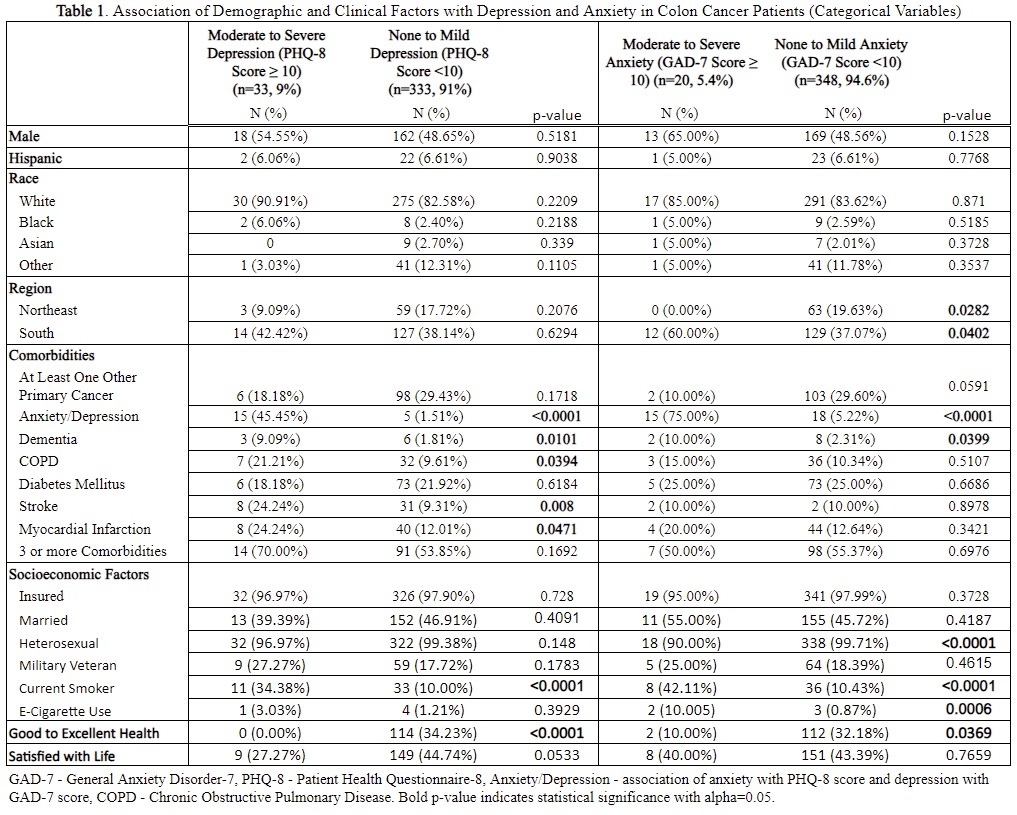
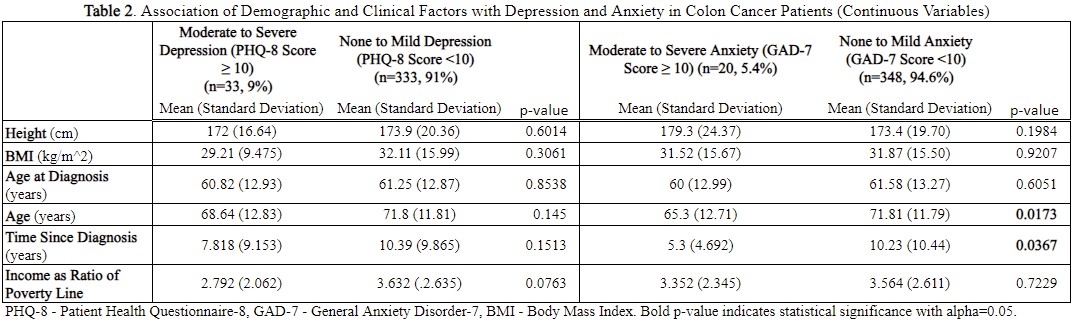
Using the National Health Interview Survey (NHIS) data from 2019-2022, we identified 764 patients that were diagnosed with CCA and 369 patients who completed the GAD-7 and/or PHQ-8 questionnaires. GAD-7 and PHQ-8 scores were calculated using individual responses. We compared patients with scores <10 (none to mild anxiety or depression) to patients with scores ≥10 (moderate to severe anxiety or depression) across various clinical and biopsychosocial factors. We performed chi-square and t-test analyses on categorical and continuous variables, respectively.
Results:
366 CCA patients completed the PHQ-8, and 368 completed the GAD-7. Among these, 33 patients (9.0%) had moderate to severe depression (PHQ-8 Score ≥ 10), and 20 patients (5.4%) had moderate to severe anxiety (GAD-7 Score ≥ 10). Significant associations with depression included anxiety (45.45%, p < 0.0001, OR=54.5), dementia (9.09%, p = 0.01, OR=5.4), stroke (24.24%, p = 0.008, OR=3.1), myocardial infarction (24.24%, p = 0.047), chronic obstructive pulmonary disorder (21.21%, p = 0.039, OR=2.5), current cigarette smoking (34.38%, p < 0.0001, OR=4.7), and self-reported health status (0%, <0.0001). For anxiety, significant factors included residence in the South (60.00%, p = 0.04) or Northeast (0%, p = 0.028), depression (75%, p < 0.0001, OR=54.5), current cigarette smoking (42.11%, p < 0.0001, OR=6.2), e-cigarette use (10.00%, p = 0.0006, OR=12.7), sexual orientation (p<0.0001), dementia (10.00%, p = 0.04, OR=4.7), self-reported health status (10.00%, p = 0.037), younger age at diagnosis (p = 0.017), and less time since diagnosis (p = 0.037).
Conclusion:
Our analysis highlights several factors that are significantly associated with the prevalence of moderate to severe anxiety or depression among CCA patients. These insights are crucial to addressing the well-being of CCA patients. Our study was limited by its retrospective and cross-sectional nature. Disease-specific characteristics such as stage at presentation and treatment were not available, nor were certain patient characteristics, such as presence of ostomy. Lastly, we were unable to determine when patients developed anxiety or depression. In the future, prospective analysis including the variables highlighted by this study should be performed.
Table 1. Association of Demographic and Clinical Factors with Depression and Anxiety in Colon Cancer Patients (Categorical Variables)
Table 2. Association of Demographic and Clinical Factors with Depression and Anxiety in Colon Cancer Patients (Continuous Variables)
Back to 2024 Abstracts