Back to 2024 Abstracts
DECISION REGRET AND SATISFACTION WITH SHARED DECISION MAKING IN PANCREATIC SURGERY
Nicholas Galouzis
*, Maria K. Fotinos, Evelyn V. Alexander, Mohammad Khreiss, Carrie Luu, Lusine Mesropyan, Taylor S. Riall
Department of Surgery, Banner - University Medical Center Tucson, Tucson, AZ
Introduction: Pancreatectomy has a significant impact on quality of life. It often does not provide long-term survival in cancer, nor does it consistently improve symptoms in benign disease. Our aim was to assess decision regret and satisfaction with the decision-making process in patients who underwent a pancreatectomy.
Methods: We administered the Brehaut Decision Regret Scale (DRS), 9-item Shared Decision-Making Questionnaire (SDM-Q-9) in addition to the European Organization for Research and Treatment of Cancer Core Quality of Life questionnaire (EORTC QLQ-C30) to all patients who underwent elective pancreatic surgery at our institution from 2021-2023. Based on prior literature, we defined regret as DRS>25. We evaluated the association between decision regret and patient demographics, time from surgery, pathology, and postoperative major complications. We evaluated SDM-Q-9 responses in patients who did and did not have regret to understand the aspects of shared decision-making that might serve as targets for improvement.
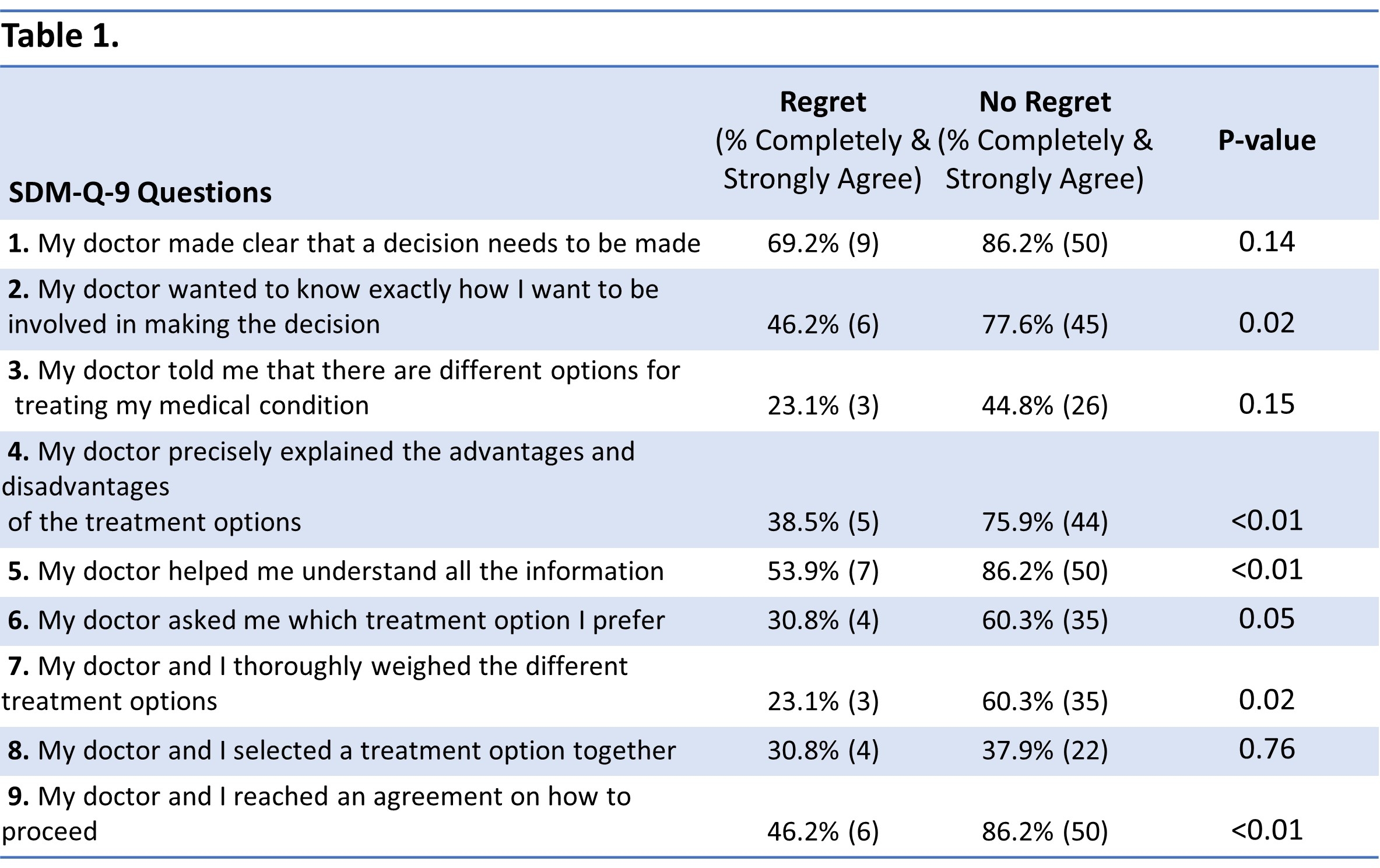
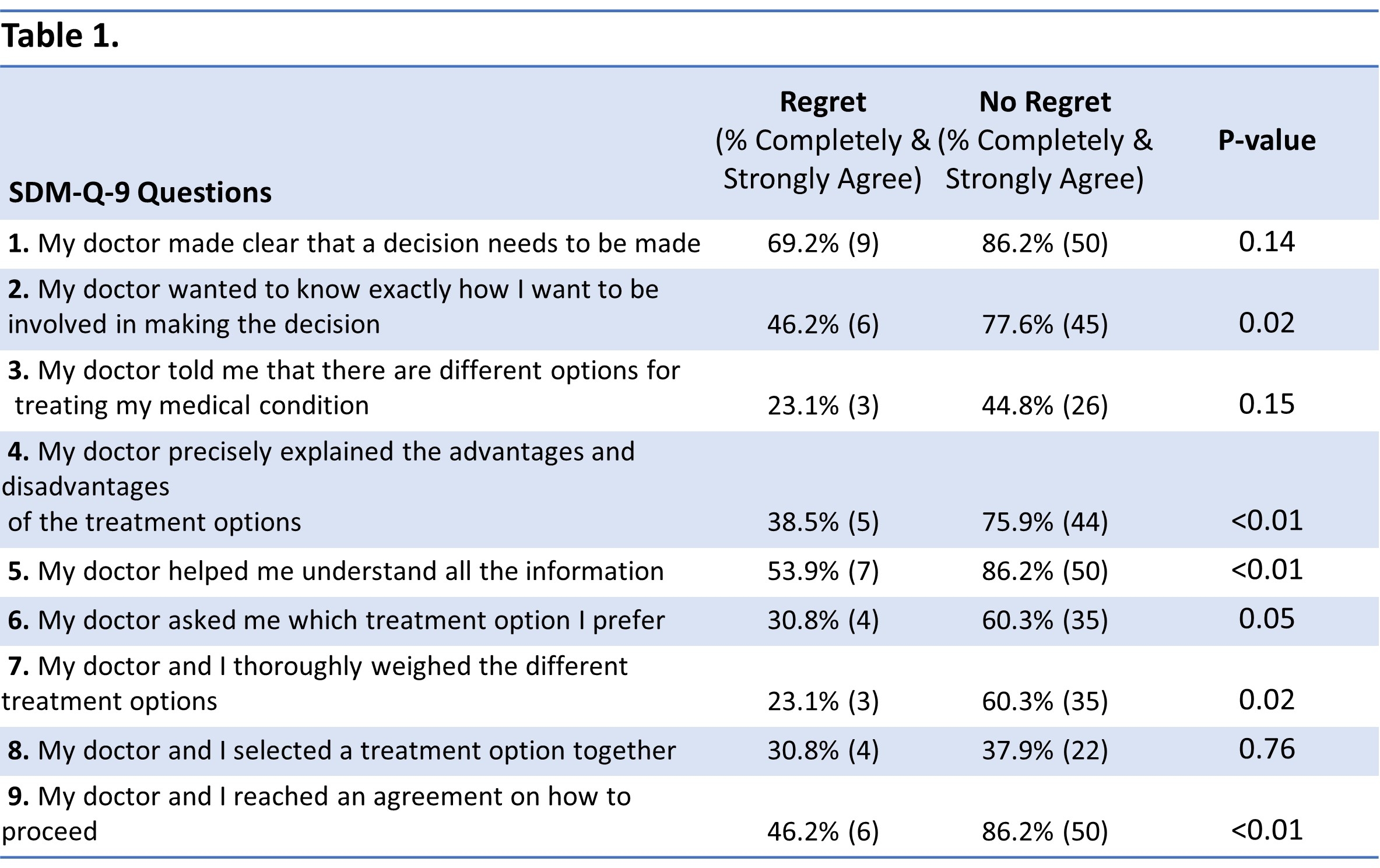
Results: 143 patients were included in this study with 71 (49.6%) completing the distributed surveys. Demographics, pathology, and major complication rates were similar between responders and non-responders. For responders, the average age was 59.9±16.1 years and 56.3% were male. 55.0% underwent pancreaticoduodenectomy. The indication for surgery was malignancy in 69.9% and benign disease in 30.1%. Decision regret after pancreatic surgery was reported in 18.3% (N=13) of patients. Patients who experienced regret were younger (50.8±18.7 vs 61.95±14.9, p=0.03). They were also more likely to have benign disease (53.9% vs 24.1%, p=0.03), to have undergone a distal pancreatectomy (76.9% vs 32.8%, p=0.02), or have experienced a major complication (53.9% vs 20.7%, p=0.01). Patients with regret had lower global health scores (57.1±20.1 vs 76.2±22.2, p<0.01) and lower social function scores (61.5±31.5 vs 77.6±22.0, p=0.03) on the EORTC QLQ-C30. Patients with regret were less satisfied with the shared decision-making process (
Table 1). Their dissatisfaction centered around not feeling they were given all treatment options and not understanding all the information including disadvantages and advantages of each treatment option. They were also less likely to feel that their surgeons did not elicit their preferences, help them weight treatment options, or come to an agreement on how to proceed together.
Conclusions: Almost one fifth of patients undergoing major pancreatic surgery experience decision regret. Younger age, distal pancreatectomy, benign indication for surgery, and major postoperative complications were associated with regret. Data from the SDM-9 highlight areas for potential improvement in shared-decision making to better inform patients and help them make decisions aligned with their goals of care.
Back to 2024 Abstracts