SOCIOECONOMIC STATUS AND ITS EFFECTS ON COLORECTAL SURGERY OUTCOMES: A SINGLE INSTITUTION STUDY
Joshua Zane*1, Molly Mounsey2, Ashar Ata1, Jonathan J. Canete1, Brian T. Valerian1, A. David Chismark1, Edward C. Lee1
1Surgery, Albany Medical College, Albany, NY; 2University of California San Francisco Fresno, Fresno, CA
Background:
Socioeconomic status (SES) has proven significant impact on colorectal cancer (CRC) outcomes. Lower SES has correlated with increased comorbidities, risk of postoperative complications, and inadequate adherence to treatment guidelines. Previous studies were limited in defining SES because of databases lacking sufficient socioeconomic variables. We utilized the CDC's Social Vulnerability Index (SVI) which contains additional information that more accurately determines SES. We hypothesize that higher SVI associates with worse clinical outcomes in CRC patients undergoing surgery at a high-volume tertiary care center.
Methods:
This is a single institution retrospective study of National Surgical Quality Improvement Program (NSQIP) data for patients aged 18 and older who underwent CRC surgery from 2013-2020. Patient zip codes were used to determine SES via the SVI database. Patients were divided into quartiles from low to high SVI (Q1-Q4). Outcomes measured included NSQIP defined morbidity, surgical site infection (SSI), extended length of stay (LOS>7), 30-day readmission. Bivariate and multivariate analysis were completed.
Results:
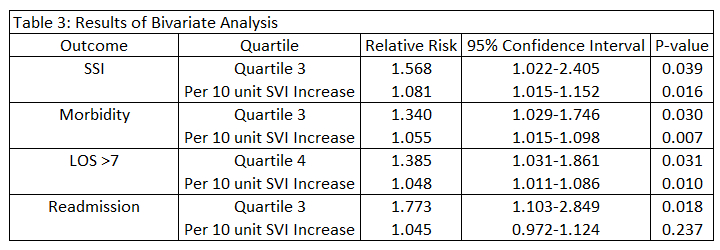
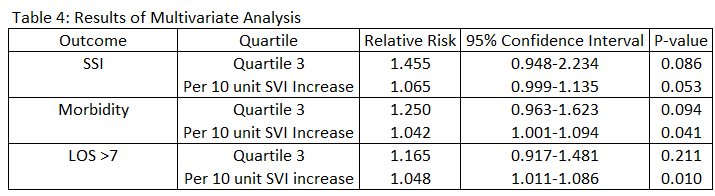
1,242 patients underwent CRC surgery during the study period. Morbidity, LOS>7, and SSI trended higher in the third and fourth quartiles but were not statistically significant. Bivariate analysis revealed a significantly increased risk of morbidity, SSI, and readmission in the third quartile, and a significantly increased LOS>7 in the fourth quartile. Continuous bivariate analysis showed that every 10 unit increase in SVI significantly increased risk for morbidity, LOS>7, and SSI. There was also a significant risk to morbidity and LOS>7 per 10 unit increase in social vulnerability on continuous multivariate analysis.
Conclusion:
This study represents a novel application of the SVI to investigate clinical outcomes using NSQIP data. Both bivariate and multivariate analysis revealed a significantly increased risk of poor clinical outcomes with higher SVI. Future application of the SVI may reveal possible interventions to improve colorectal and other surgical outcomes.
Back to 2023 Abstracts


