CLINICAL OUTCOMES FOLLOWING ROBOTIC ABDOMINAL WALL RECONSTRUCTION FOR VENTRAL HERNIAS USING RESORBABLE BIOSYNTHETIC MESH
Alexandra C. Skoczek*1, Patrick W. Ruane2, Dennis L. Fernandez3
1Edward Via College of Osteopathic Medicine - Auburn Campus, Auburn, AL; 2Edward Via College of Osteopathic Medicine - Carolinas Campus, Spartanburg, SC; 3Crestwood Medical Center, Huntsville, AL
Background The open approach and the minimally invasive laparoscopic approach have been the mainstay for ventral hernia repair in the United States. While these techniques are successful in repairing ventral hernias, they tend to have high rates of surgical site occurrences (SSO), recurrence rates, and prolonged hospital length of stay (LOS) (>4 days) in patients with modifiable comorbidities (MCMs). Compared to open and laparoscopic hernia repairs, robotic hernia repairs have shown to have better postoperative outcomes, however, no studies have been conducted evaluating MCMs effects on these outcomes. We hypothesized that there would be no difference in postoperative outcomes (SSO, recurrence rate, and prolonged LOS) in patients with and without MCMs following robotic transversus abdominis release (TAR) with resorbable biosynthetic mesh underlay for primary ventral hernia repair. Methods A retrospective review of medical records for patients who underwent robotic TAR with resorbable biosynthetic mesh underlay for ventral hernia repair between 2015 and 2022 performed by a single surgeon was conducted. Three groups were analyzed (patients with 0, 1, and 2+ MCMs) followed by a breakdown of comorbidity type and combinations of comorbidities. The three MCMs documented include diabetes, smoking, and obesity (BMI > 30 kg/m2). Results A total of 334 subjects met the inclusion criteria for SSO and prolonged LOS analysis. Of those, 16.8% had no MCM, 56.1% had 1 MCM, and 27% had 2+ MCMs. No significant difference in SSO was seen between the 3 groups, however, having 2+ MCMs was significantly associated with increased odds of SSO (odds ratio 3.25, p=.019). When the groups were broken down, only having a history of diabetes and obesity was associated with significantly increased odds of SSO (odds ratio 3.54, p=.02). Though there was a difference between the three groups, none showed a significantly increased odds of prolonged LOS. A total of 175 subjects met the inclusion criteria for recurrence at 36-month follow-up analysis. Of those, 21.1% had no MCM, 48% had 1 MCM, and 30.9% had 2+ MCM. There was no significant difference seen in recurrence rate or significant increase in odds of recurrence between the 3 groups or between the different MCMs and combinations of MCMs. Conclusion The presence of 2+ MCMs significantly increases the odds of SSO, specifically in patients who have a history of diabetes and obesity. However, the presence of any number of comorbidities (0 MCM, 1 MCM, or 2+ MCM) was not associated with increased odds of prolonged length of hospital stay or recurrence after 36 months. These findings suggest that the robotic TAR with resorbable biosynthetic mesh underlay for primary ventral hernia repair may be a preferred method of ventral hernia repair in patients with MCM to decrease adverse postoperative outcomes.

Surgical site occurence (SSO) and length of stay (LOS) analysis
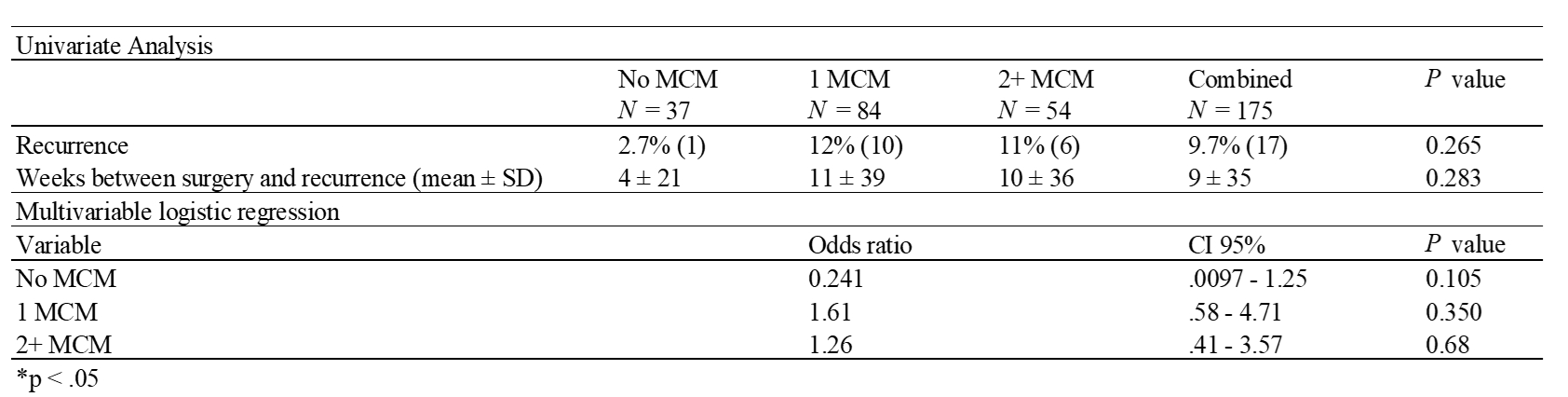
Recurrence at 36 month follow up analysis
Back to 2023 Abstracts


