A COMPARISON OF CLINICAL AND COST OUTCOMES AFTER PANCREATECTOMY AT A SAFETY-NET HOSPITAL USING THE VIZIENT CLINICAL DATA BASE
Keouna Pather*, Erin M. Mobley, Christina Guerrier, Rhemar Esma, Ziad Awad
Surgery, University of Florida College of Medicine - Jacksonville, Jacksonville, FL
Objective: Pancreatectomies are technically challenging procedures frequently associated with morbidity and mortality. Nonetheless, pancreatectomies are the only potentially curative treatment for pancreatic cancer. The aim of this study is to compare the clinical and cost outcomes of patients undergoing pancreatectomy for treatment of pancreatic cancer at our institution against national benchmarks of large, specialized complex care medical centers (LSCMCs) and safety-net hospitals (America's Essential Hospitals, AEHs).
Methods: The Vizient Clinical Data Base was queried for all participating institutions performing any type of pancreatectomy for pancreatic cancer for adults over the age of 18 from 2018-2020. Institution-level clinical and cost outcomes were compared across our institution, LSCMCs, and AEHs. Clinical outcomes included hospital length of stay (LOS) index, 30-day mortality index, case mix index (CMI), and percentage of 30-day readmissions. Cost outcomes comprised the direct cost index. LOS, mortality, and direct cost indices were defined as the ratio of observed values to expected values, derived from the Vizient comparison hospitals. Indices with a value greater than one indicated the observed value was greater than the expected comparison value for that measure.
Continuous variables were summarized as weighted means and standard deviation. Continuous measures were analyzed by the two-sample t-test or Mann-Whitney U test, as appropriate. P-values with ?<0.05 defined statistical significance.
Results: A total of 78 LSCMCs and 52 AEHs performed 6,795 pancreatectomies from 2018-2020. Our institution performed a total of 90 pancreatectomies during this period.
LOS index was below national benchmarks at our institution (1.08-0.82), LSCMCs (0.91-0.85), and AEHs (0.94-0.93), with an increasing CMI at our institution (3.33-4.20) from 2018-2020. The mortality index declined at our institution (5.07-0.00) below national benchmarks compared to LSCMCs (1.23-1.29) and AEHs (1.19-1.45). 30-day readmissions were lower at our institution (6.25-10.26%) compared to LSCMCs (17.62-16.83%) and AEHs (18.93-15.51%). Direct cost index at our institution declined (1.00 to 0.67) below the benchmark compared to LSCMCs (0.90-0.93) and AEHs (1.02-1.04).
Conclusion:
From 2018-2020, clinical and cost outcomes after pancreatectomies for pancreatic cancer at our safety-net hospital are comparable to peer LSCMCs and AEHs. These outcomes have improved, exceeding national benchmarks despite an increasing CMI over this 3-year period. These findings are of particular importance given the growing reimbursement constraints coupled with the strain of the COVID-19 pandemic on the health care system. This study highlights the role of LSCMCs and safety-net hospitals in providing high-quality care to a medically underserved population requiring complex surgery.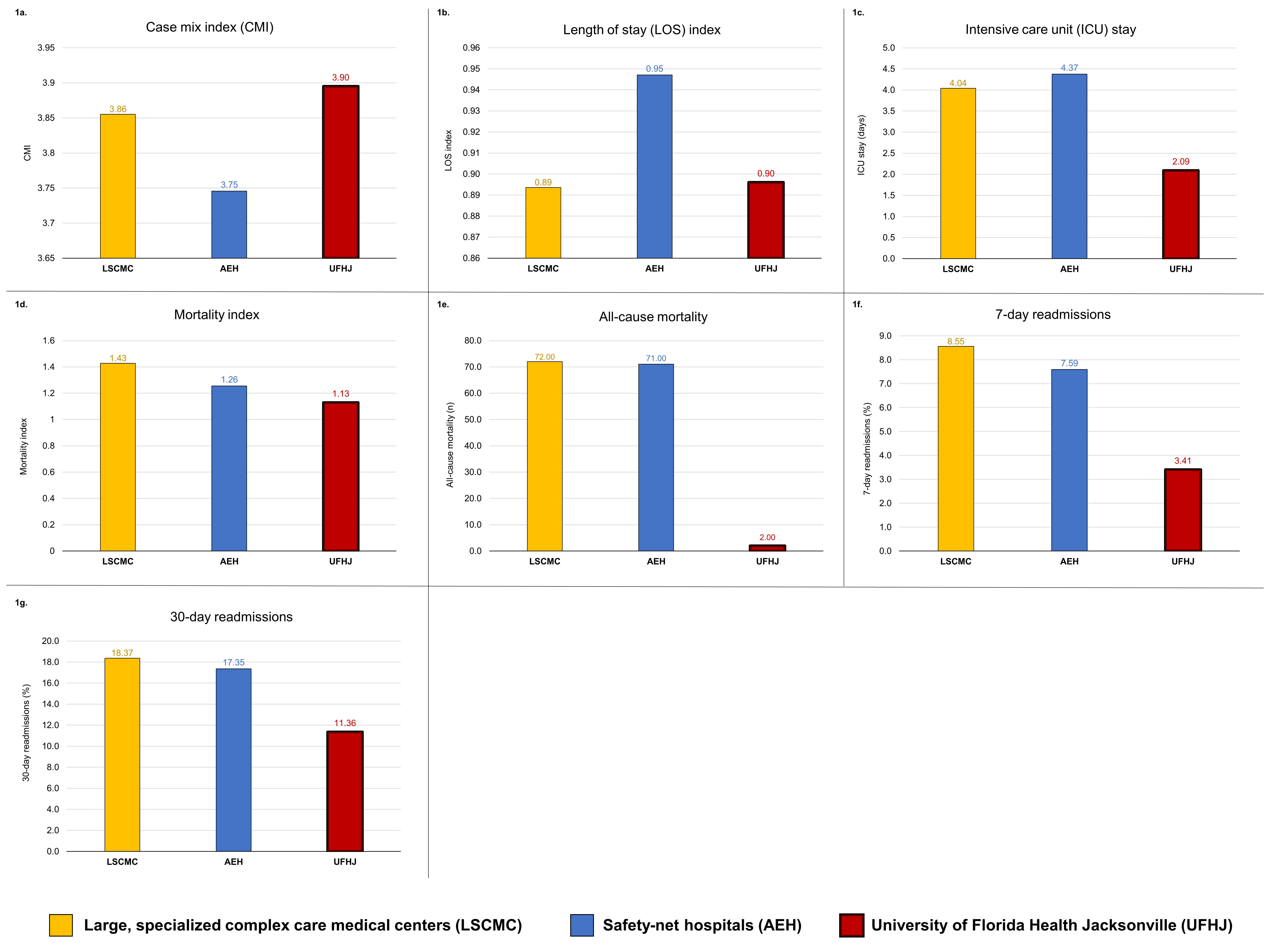
Clinical outcomes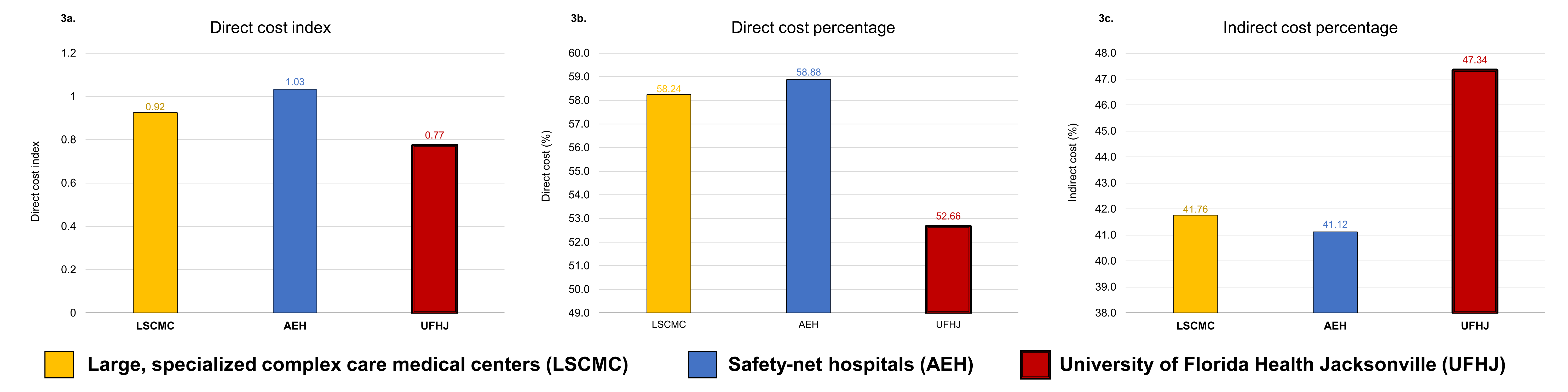
Cost outcomes
Back to 2022 Abstracts
