INCREASED ODDS OF OSTEOPOROSIS-RELATED FRACTURES IN PATIENTS WITH HISTORY OF ROUX-EN-Y GASTRIC BYPASS
Paul T. Kröner1, Alfred D. Nelson*1, Klaus E. Monkemuller1, Marco A. D'Assuncao1, Juan P. Gutierrez1, Giovani Schwingel1, Frank Lukens1, Christopher C. Thompson2
1Mayo Clinic's Campus in Florida, Jacksonville, FL; 2Brigham and Women's Hospital, Boston, MA
Introduction
As the epidemic of obesity continues to evolve, obesity surgery has become an important means to address the issue. Procedures that bypass a portion of the small bowel, such as Roux-en-y gastric bypass (RYGB), have been associated with mineral and nutritional deficiencies. Calcium absorption, essential for bone mineral density, may be impaired, placing patients at risk of osteoporosis in the long term. The aim of this study was to assess osteoporosis-related fractures in patients with and without history of RYGB.
Methods
Retrospective, observational study using the National Inpatient Sample (NIS) 2018. All patients with ICD10CM codes for osteoporosis-related fractures were included. The cohort was matched for age and stratified depending on whether patients had history of having had bariatric surgery or not. The primary outcome was the odds of osteoporosis-related fractures in patients with history of bariatric surgery compared to patients without history of bariatric surgery, substratified by anatomical location of the fracture. Multivariate regression analyses were used to adjust for age, gender, Charlson Comorbidity Index, income by patient zip code, hospital region, location, size and teaching status.
Results
A total of 57,295 patients were admitted for osteoporosis-related fractures, out of which 520 had a history of RYGB and 60 had history of SG. The mean age in patients with history of RYGB was 66 years and 96.15% were female. For the primary outcome, patients with history of RYGB displayed increased odds of osteoporotic fractures (aOR:1.19, p=0.05) compared to patients with no history of RYGB. These associations were evident for femoral fractures (aOR: 1.37, p=0.03) and leg fractures (aOR: 2.71, p<0.01).
Conclusions
In conclusion, patients with a history of RYGB have associated increased odds of osteoporosis-related fractures compared to age-matched patients with no history of RYGB. This was especially seen for femoral and leg fractures. This association was not seen in patients with SG. This study highlights the importance of long-term follow-up and preventive medicine in patients who have a history of RYGB. Further prospective studies should focus on eliciting specific factors that may contribute to the progression of osteoporosis in patients with RYGB.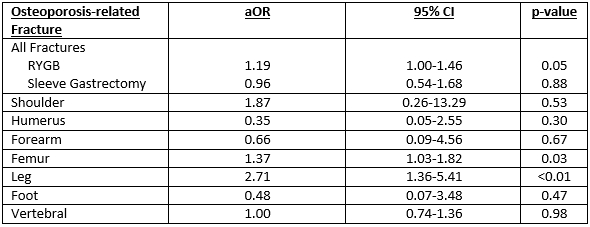
Table 1 – Adjusted odds ratios of osteoporosis-related fracture for patients with history of bariatric surgery compared to patients without history of bariatric surgery.
Back to 2022 Abstracts
