UTILIZATION AND HEALTHCARE DISPARITIES IN TREATMENT OF DIVERTICULITIS
Laxmi P. Dongur, Fernando Lambreton*, Elizabeth O'Daniel, Uma R. Phatak
Surgery, The University of Texas Medical Branch at Galveston, Galveston, TX
Introduction:
Diverticular disease is a common pathology in the United States. Of those with diverticular disease, approximately 4 to 15 % develop diverticulitis. The care of patients with diverticulitis is often multidisciplinary and can be disjointed. The aim of our study is to analyze healthcare utilization among patients with diverticulitis who receive resection.
Methodology:
We performed a single center retrospective chart review of patients over the age of 18 years who were diagnosed with diverticulitis either through imaging or tissue analysis between the years of 2014 and 2019. We used CPT codes to identify patients who underwent a colorectal resection for diverticulitis. Data were gathered regarding demographics, socioeconomic status, comorbidities, number of CT scans, number of ER visits, type of operation, operative approach, and post-operative outcomes. All analyses were performed with STATA 14 (College Station, TX).
Results:
We identified 103 patients of which 56.2% were male and 89.5% were Caucasian. The median age in years was 59.2 (IQR 50.5, 68.9) and the median BMI was 28.8 (IQR 24.9, 32.6). The median number of CT scans was 2 (IQR 1, 3) and the median number of ER visits was 1 (IQR 1, 2). Less than half of the cohort had more than 1 attack prior to surgery (44.3%). The mean number of er visits was not significantly different between the elective and non-elective groups (1.7 days vs 1.8 days, p=0.85). The median hospital length of stay in days was 5 (IQR 3, 9.5). The most common operative approach was open 46.6% followed by robotic 34%, and 75% of operations were elective. The mean length of stay was significantly shorter for those who received elective surgery compared to non-elective surgery (5.5 days vs. 13.8 days, p<0.001). Compared to people with public and no insurance, patients with private insurance had more episodes of diverticulitis (4.3 vs 2.5 vs 2.3, p=0.023) before resection, and these were more likely to be treated as outpatient (3 vs 1.1 vs 1.1, p=0.004). Length of stay was higher for patients with no insurance than for public or private insurance (14.3 vs 8.1 vs 5.8, p=0.005). Patients with public/no insurance were more likely to have an emergency procedure (18% vs 6.9%, p= 0.027).
Conclusion:
Most operations for diverticulitis were elective and the number of CT scans and ER visits per patient was lower than expected. However, lack of private insurance resulted in more emergency surgery and length of stay. There was not a significant difference in ER utilization in the elective vs. non-elective group. Having a non-elective surgery was associated with a significantly longer hospital stay. Further study is needed to identify barriers to receiving an elective operation.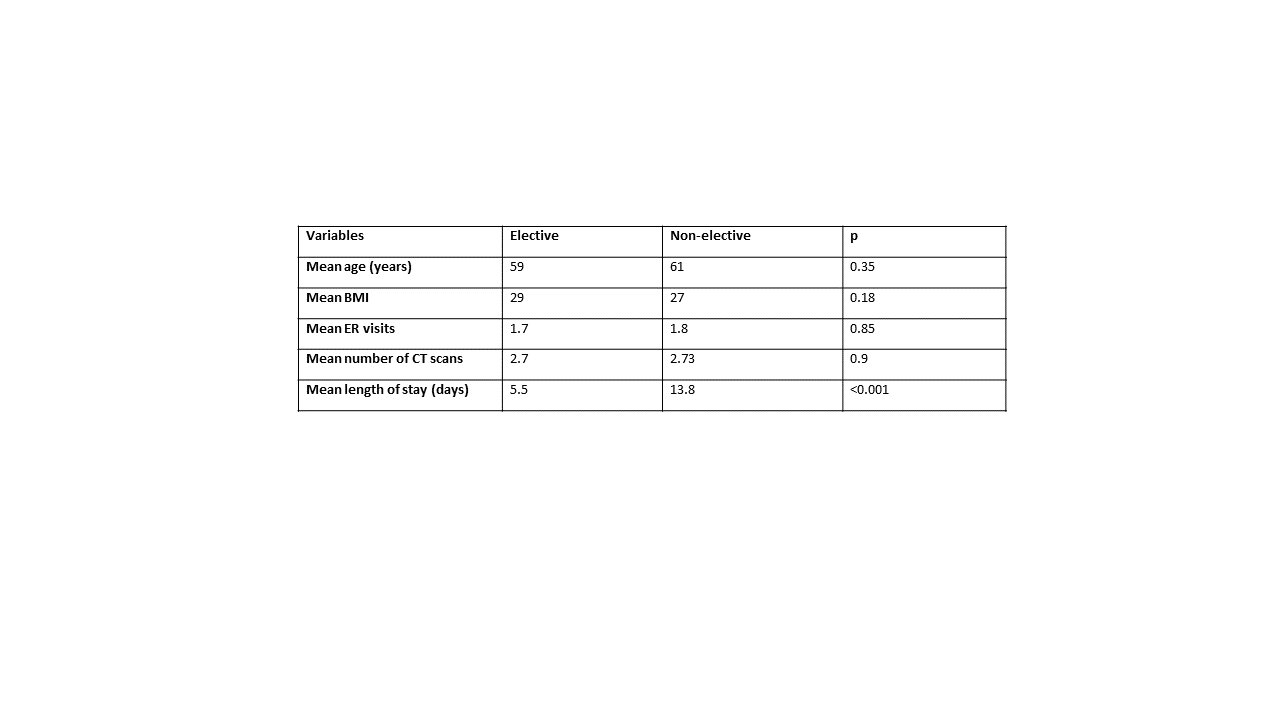
Table 1. Comparison between elective and non-elective cases.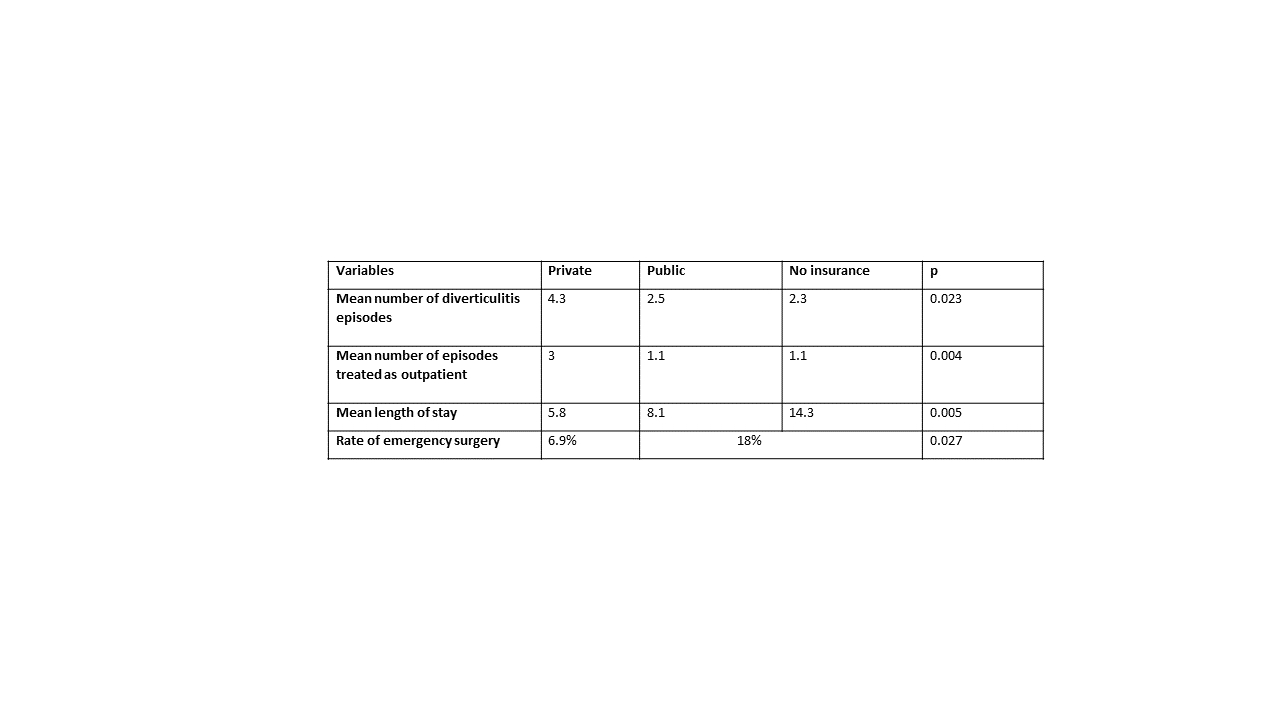
Table 2. Comparison between private and public insurance.
Back to 2022 Abstracts
