AN AGE-STRATIFIED ANALYSIS OF EARLY POSTOPERATIVE MORTALITY AMONG PATIENTS WITH COMMON GASTROINTESTINAL MALIGNANCIES
Alexander W. Loftus*, Jonathan J. Hue, Mohamedraed Elshami, Richard S. Hoehn, Luke Rothermel, John Ammori, Jeffrey Hardacre, Jordan M. Winter, Lee M. Ocuin
General Surgery, University Hospitals Cleveland Medical Center, Univeristy Heights, OH
Introduction
The average age of the population has increased, as have the number of major cancer procedures performed in the elderly (?80yrs), who have limited physiologic reserve and are at increased risk for postoperative mortality. We have previously reported that patients ?80yrs have are at significant risk of mortality between 30-90d following pancreatoduodenectomy (PD). Our aim was to assess early postoperative mortality following hepato-pancreato-biliary (HPB) and gastrointestinal (GI) procedures for common malignancies stratified by age.
Methods
The National Cancer Database (2004-2017) was queried for patients who underwent a resection for GI (esophageal, gastric, colon, rectum) or HPB (pancreatic, intrahepatic bile duct, gallbladder, hepatic) cancers. We compared early postoperative mortality (?30d and 30-90d) stratified by age (60-79 vs. >80yrs), using multivariable logistic regression to adjust for clinicodemographic and pathologic variables.
Results
A total of 665,079 patients were included: 73% were 60-79yrs and 27% were ?80yrs. The overall mortality rates ?30d and between 30-90d for patients 60-79yrs were 2.5% and 2.2%, respectively. For patients ?80yrs, the rates were 7.2% and 5.2% (p<0.001). Elderly patients experienced the highest rates of 30-90d mortality following major resection for gallbladder cancer (10%), esophagectomy (9%), total gastrectomy for gastric cancer (9%). All 30-90d mortality rates were ?5.5% for patients aged 60-79yrs regardless of diagnosis or procedure. On multivariable analysis, age ?80yrs was associated with an increased likelihood of death between 30-90d (OR 2.7, p<0.001). Treatment at an academic center (OR 0.86, p<0.001) and receipt of neoadjuvant chemotherapy (OR 0.76, p<0.001) were associated with a reduced likelihood of death between 30-90d. Using PD as a reference, esophagectomy, total gastrectomy, major hepatectomy (for intrahepatic cholangiocarcinoma), and major resection for gallbladder cancer were all associated with an increased likelihood of death between 30-90d (OR 1.3-1.6, p<0.05 for all, Figure). Conversely, major hepatectomy for hepatocellular carcinoma, distal pancreatectomy, partial colectomy (colon or rectosigmoid junction cancers), total colectomy (rectosigmoid junction cancer), and proctectomy for rectal cancer were all associated with a reduced likelihood of postoperative mortality between 30-90d (OR 0.4-0.9, p<0.04 for all, Figure).
Conclusion
Elderly patients suffer higher postoperative mortality after major cancer surgery relative to a younger cohort. This mortality rate is associated with both the procedure and the malignancy. The underlying causes of mortality are unclear and likely multifactorial, but these data are important to contextualize when counseling elderly patients on their treatment options.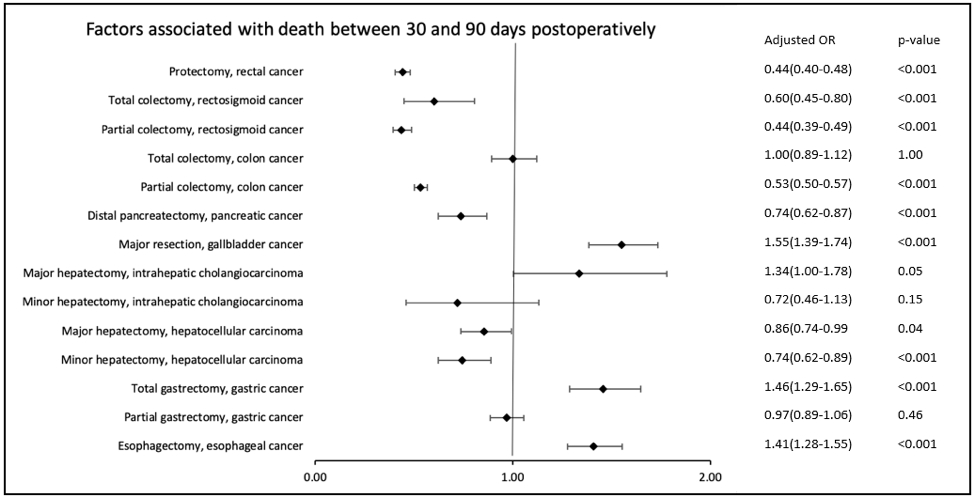
Back to 2022 Abstracts
