PROGNOSTIC IMPLICATIONS OF MARGIN STATUS IN ASSOCIATION WITH SYSTEMIC TREATMENT IN PATIENTS WITH RESECTION OF COLORECTAL LIVER METASTASES
Omeed Moaven*1, Cristian D. Valenzuela1, Gregory B. Russell1, Tan To Cheung2, Carlos U. Corvera3, Andrew D. Wisneski3, Charles Cha4, John Stauffer5, Nico Del Piccolo5, Perry Shen1
1Department of Surgery, Wake Forest University School of Medicine, Winston-Salem, NC; 2The University of Hong Kong Li Ka Shing Faculty of Medicine, Hong Kong, Hong Kong; 3UCSF Medical Center, San Francisco, CA; 4Hartford HealthCare, Hartford, CT; 5Mayo Clinic in Florida, Jacksonville, FL
Background: Despite significant improvements in the outcomes of patients with colorectal liver metastasis (CLM), there is still a lack of consensus on the sequence of multimodality treatment and the clinical significance of positive margin after hepatectomy in association with systemic therapy. In this study, we investigate the impact of margin status after CLM resection on outcomes in patients who received neoadjuvant treatment and those who undergo upfront resection.
Methods: An international collaborative retrospective database of CLM patients who underwent surgical resection between 2000 to 2018 was used. Patients who received tumor ablation, had extrahepatic disease at the time of diagnosis, or had repeat hepatectomy were excluded. Proportional hazards regression models were created for single and multivariable models to assess the relationship between independent measures and overall survival (OS). OS was compared in patients with negative margin (R0) vs. positive margin (R1) in the whole cohort and after stratification based on the timing of systemic therapy.
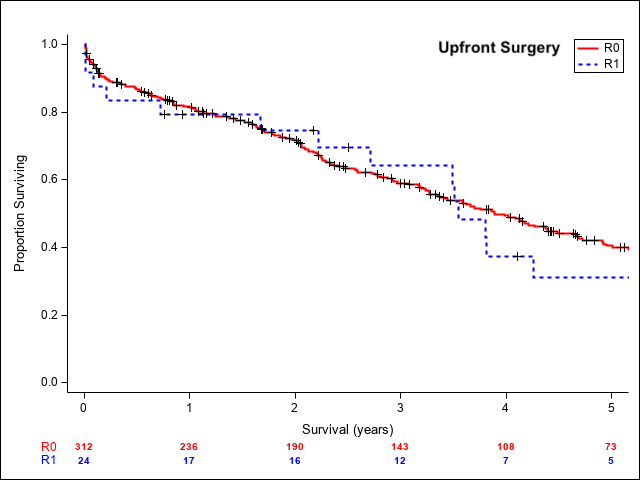
Results: A cohort of 689 patients met the inclusion criteria for this study. Positive margin was observed in 10.4% of the patients (72/689), with no significant difference between patients who received neoadjuvant (39/344) compared to upfront surgery (33/345). Positive margin was associated with worse OS in the neoadjuvant group (median OS: 51.8m for R0 vs. 26.0m for R1; HR:2.34, 95%CI:1.39-3.95, p value=0.005). In the patients who underwent upfront surgery, positive margin was not associated with OS. (median OS: 46.7m for R0 vs. 42.6m for R1; HR:1.10, 95%CI:0.66-1.84, p value=0.758). When the patients with positive margin in each group were stratified by adjuvant treatment, there was no significant difference in the neoadjuvant group (median OS: 28.6 for adjuvant treatment vs. 20.6m for no adjuvant treatment; HR:0.62, 95%CI:0.27-1.42, p value=0.260), while in the upfront surgery group with positive margin, adjuvant treatment was associated with significant improvement in overall survival (median OS: 42.6 for adjuvant treatment vs. 25.0m for no adjuvant treatment; HR:0.22, 95%CI:0.07-0.67, p value=0.007).
Conclusion: Positive margin is associated with worse outcomes in the patients who receive neoadjuvant treatment with no significant improvement with the addition of adjuvant therapy, likely representing a poor response to chemotherapy in the setting of aggressive tumor biology. Positive margin did not impact overall survival in patients with upfront surgery who received postoperative chemotherapy.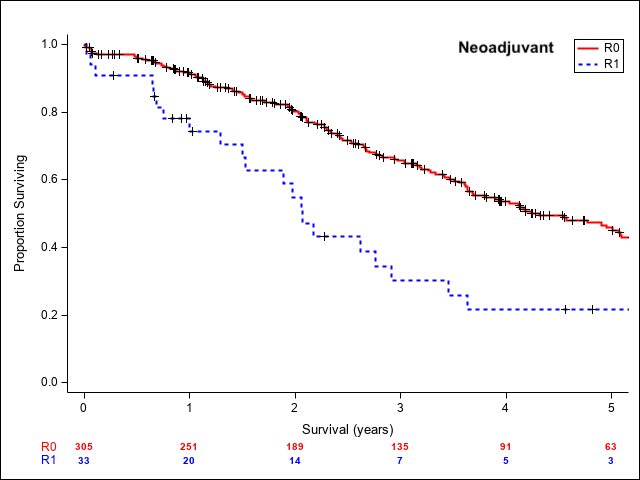
Back to 2022 Abstracts
