PRE-OPERATIVE GHRELIN LEVELS MAY IMPROVE ACCURACY OF WEIGHT LOSS PREDICTION FOLLOWING ROUX-EN-Y GASTRIC BYPASS SURGERY
Mehran Karvar*, Hassan Aliabarian, Andrei Moscalu, Cullen F. Roberts, Yingjia Chen, Eric G. Sheu, Ali Tavakkoli
Surgery, Brigham and Women's Hospital, Boston, MA
Introduction: Bariatric surgery including Roux-en-Y Gastric Bypass (RYGB) is the most effective treatment for morbid obesity. Predicting weight loss following RYGB remains a clinical challenge. The American College of Surgeons Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) has developed a calculator based on its large patient dataset to predict anticipated weight loss and help patients' make informed decisions regarding their surgery. The accuracy of their prediction model is variable. We propose addition of biological markers to improve the accuracy of prediction models for weight loss after RYGB.
Methods: We used the MBSAQIP online calculator to predict weight loss of 95 laparoscopic RYGB patients (%Predicted-TWL) in comparison to their actual total body weight loss at 1 year (%Actual-TWL). Two subgroups of patients were identified: 1) Good Weight Loss group in which %Actual-TWL was greater than by 5% from %Predicted-TWL (mean %Actual-TWL of 42.81 ± 4.38% vs 33.70 ± 2.58 %Predicted-TWL), and 2) Poor Weight Loss group in which %Actual-TWL was less than by 5% from %Predicted-TWL (mean %Actual-TWL of 24.97 ± 5.02% vs 34.04 ± 1.98 %Predicted-TWL). Serum fasting pre-operative hormone levels, including glucagon, leptin, and ghrelin were measured and compared between the patients of these subgroups.
Results: Table 1 summarizes group demographics. Among 95 patients, 23.2% had Good Weight Loss, while 24.2% had Poor Weight Loss, as compared with their %Predicted-TWL. Subgroup analysis showed that patient demographics and baseline characteristics were similar between these groups. However, for measured hormones regulating weight, pre-operative Ghrelin levels were significantly higher in the Good Weight Loss subgroup vs. Poor Weight Loss subgroups (65.10 ± 22.88 pg/mL vs 44.36 ± 12.20 pg/mL; p=0.0006; Table 1), suggesting an important role for this hormone in driving post-operative outcomes.
Conclusions: Current bariatric surgery weight loss calculators inaccurately predict patient weight loss by at least 5% TWL in nearly half of the patients, limiting their value. We find that differences in pre-operative ghrelin levels, and not patient demographic factors, are associated with failure of the MBSAQIP weight loss predictor. Addition of pre-operative biological markers has the potential to improve accuracy of weight loss prediction calculators and should be measured to help assist patients and surgeons in clinical decision-making.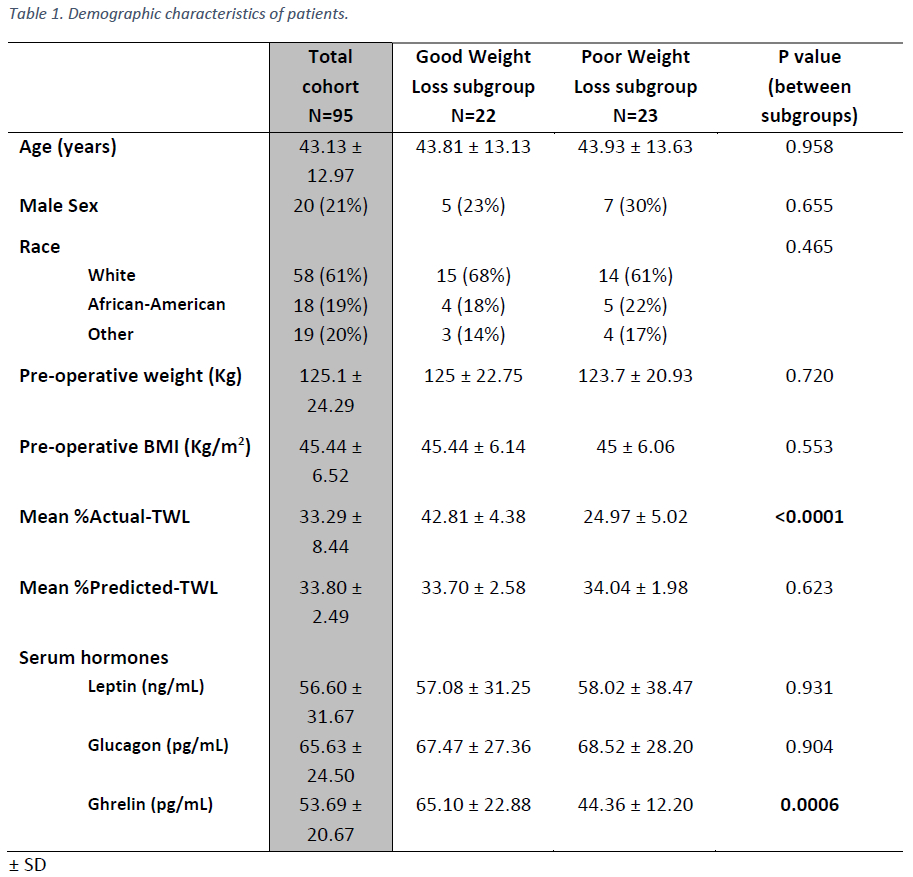
Back to 2022 Abstracts
