DOES GOAL-DIRECTED FLUID MANAGEMENT DURING PANCREATODUODENECTOMY PREVENT DELAYED GASTRIC EMPTYING?
Alexandra M. Roch*, Rachel C. Kim, James Butler, Trang K. Nguyen, Eugene P. Ceppa, Nicholas J. Zyromski, C. Max Schmidt, Attila Nakeeb, Michael G. House
Indiana University School of Medicine, Indianapolis, IN
Background: Delayed gastric emptying (DGE) requiring nasogastric decompression is the most common complication following pancreatoduodenectomy in up to 20% of patients. Although not life threatening, DGE is associated with prolonged hospital stay and represents a major economic burden.
We sought to develop an easy risk prediction tool for DGE featuring pre- and intraoperative assessment.
Methods: Patients who underwent pancreatoduodenectomy at a single academic center from 2015 to 2019 were included. Univariable and multivariable logistic regression determined pre- and perioperative predictors of DGE. Receiver operating curves were used to evaluate the optimal cut-off value for continuous variables.
Results: Delayed gastric emptying occurred in 105 of 645 patients (16.3%) and was associated with a significantly longer hospitalization (21 vs. 9 days, p<0.0001). During multivariable analysis, preoperative severe COPD and soft pancreatic gland texture were independently associated with DGE. Large volume intraoperative fluid resuscitation (4160mL vs. 3620mL, p=0.0005), regardless of the estimated blood loss (525mL vs. 441mL, p=0.12), was associated with DGE. These three factors were used to generate a DGE predictive score, and ranked for pancreatic texture (1 to 3, hard to soft), COPD (1) or absent (0), and total perioperative intravenous fluids (£3300mL (0) vs. >3300mL (1)). Increases in DGE predictive score value were associated with increased risk for DGE (Figure), with an excellent correlation coefficient R2 (0.96). Patients with a score of 1/5 had a 4% risk of developing DGE, while DGE occurred in 42% of patients with a score of 5/5.
Conclusion: This large series describes an easy score to predict DGE after pancreatoduodenectomy. This novel tool will help better adjust peri- and postoperative practices. The liberal use of intraoperative fluids seems to play a central part in the development of DGE, thus goal directed fluid therapy, as already used during hepatectomy, should be strongly considered during pancreatoduodenectomy, especially in patients with soft glands.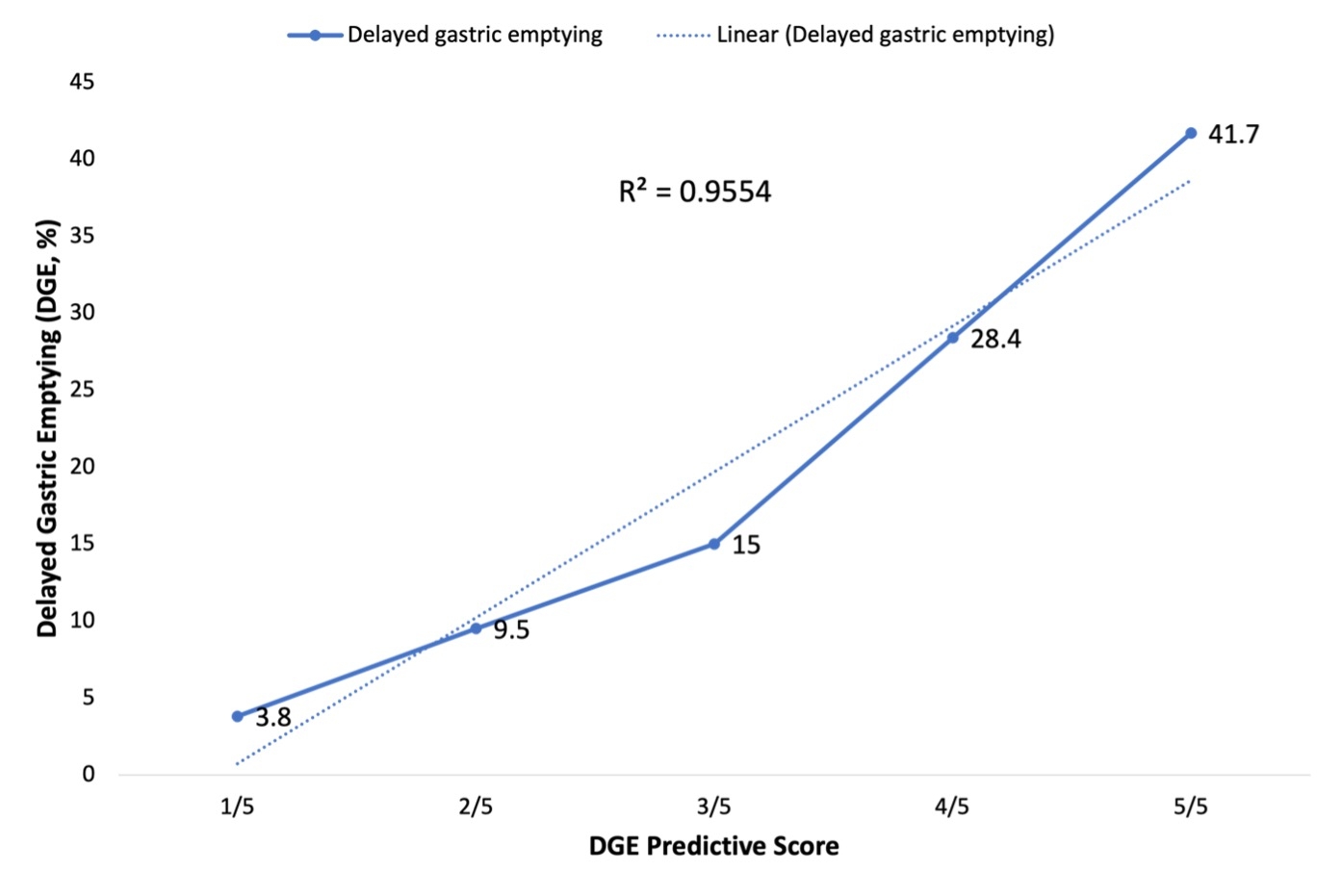
Back to 2022 Abstracts
