LIMITATIONS OF AUTOMATED ELECTRONIC MEDICAL RECORD (EMR) VENOUS THROMBOEMBOLISM (VTE) PROPHYLAXIS ADVISORS IN BENIGN FOREGUT SURGERY
Nada Mustafa*1, Clarissa Hoffman1, Sylvestre Pineau1, Raymar Turangan1, Pavel Levin2, Farzaneh Banki1, Shinil K. Shah1
1Surgery, The University of Texas Health Science Center at Houston John P and Katherine G McGovern Medical School, Sugar Land, TX; 2The US Oncology Network, The Woodlands, TX
Background: VTE prophylaxis risk assessment tools can be cumbersome and have sporadic use. We aim to assess the usage/accuracy of an automated EMR VTE prophylaxis scoring system (Caprini score, CS).
Methods: We reviewed 424 patients who underwent minimally invasive hiatal hernia repair (HH, n=331) and sleeve gastrectomy (SG, n= 93). All patients had sequential compression devices (SCD) and preoperative prophylactic dose of heparin/enoxaparin ordered (PREOP). VTE events were assessed in the entire study population. In 193 sequential patients (100 HH, 93 SG), EMR and manually calculated CS were evaluated, and patients were stratified by risk (Table 1). The rate of PREOP and post-operative pharmacologic prophylaxis (POPP) were assessed in the sequential cohort. Values are presented as median (interquartile range).
Results: Demographics, clinical data, CS, and risk categories based on CHEST guidelines are included in Table 2.
HH: An automated CS was documented in 11/100 (11.0%) patients; CS was 5.0 (3.0-7.5). When manually calculated, CS was 7.0 (6.0-7.0). The documented score was accurate in 1/11 (9.1%) patients with a discrepancy of 2.0 (1.5-3.5). This would have changed the recommended dose in 4/11 (36.4%) patients. HH cohort CS are presented in Table 2. All patients received SCDs and 97% received PREOP. None received extended post-discharge POPP. Deep vein thrombus (DVT) occurred in 1 (0.3%) patient (CS 7) who received PREOP.
SG: An automated CS was documented in 87/93 (93.5%) patients; CS was 2.0 (1-3). When manually calculated, CS was 4 (4-5). The documented score was accurate in 7/87 (8.0%) patients with a discrepancy of 2 (2-3). This would have changed the recommended dose in 22/87 (25.2%) patients. SG cohort CS are presented in Table 2. All patients received SCDs and 78% received PREOP. 95.7% received POPP. 6 (6.4%) patients received extended anticoagulation (based on CHEST guidelines in 1/6 patients). VTE events occurred in 3 (3.2%) patients (1 with DVT (CS 2) did not receive PREOP, but received POPP; 1 with pulmonary embolus (CS 10) received PREOP and was on postoperative therapeutic heparin; 1 with mesenteric vein thrombus (CS 4) received both PREOP/POPP).
Conclusion: Automated EMR based VTE advisors do not capture all patients admitted to the hospital and their usage is limited in outpatient surgery. They do not always provide clear preoperative and extended postoperative guidelines for VTE prophylaxis. There is a clinically relevant discrepancy between automated and manually calculated scores. Simplified clinical VTE risk scoring systems that rely on uniformly abstractable data by EMR systems without the need for manual input and tailored to the specific patient population/surgery type are needed.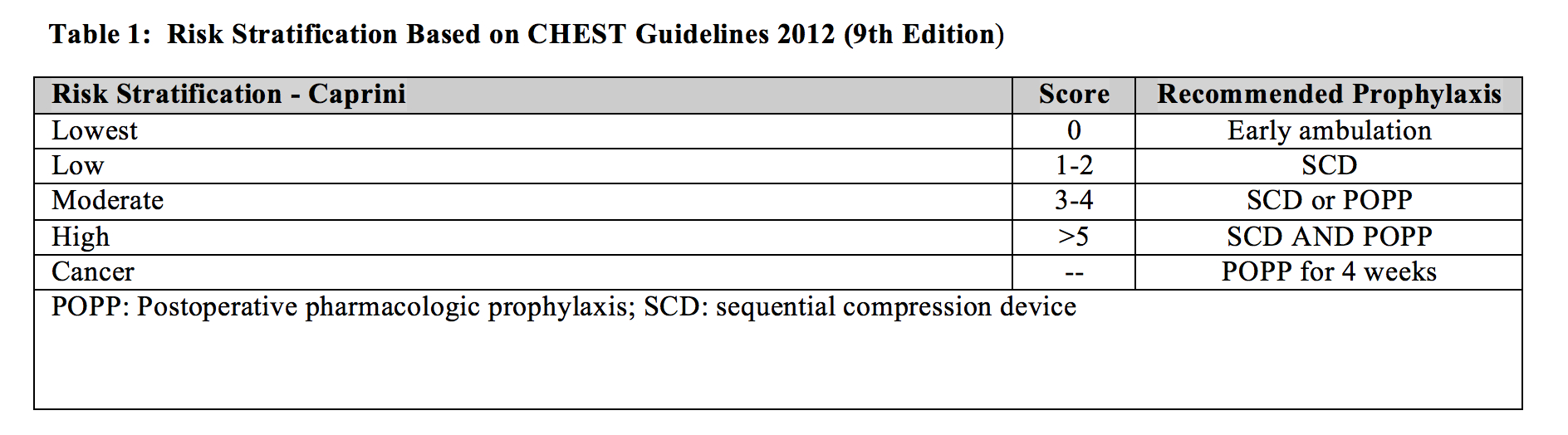
Table 1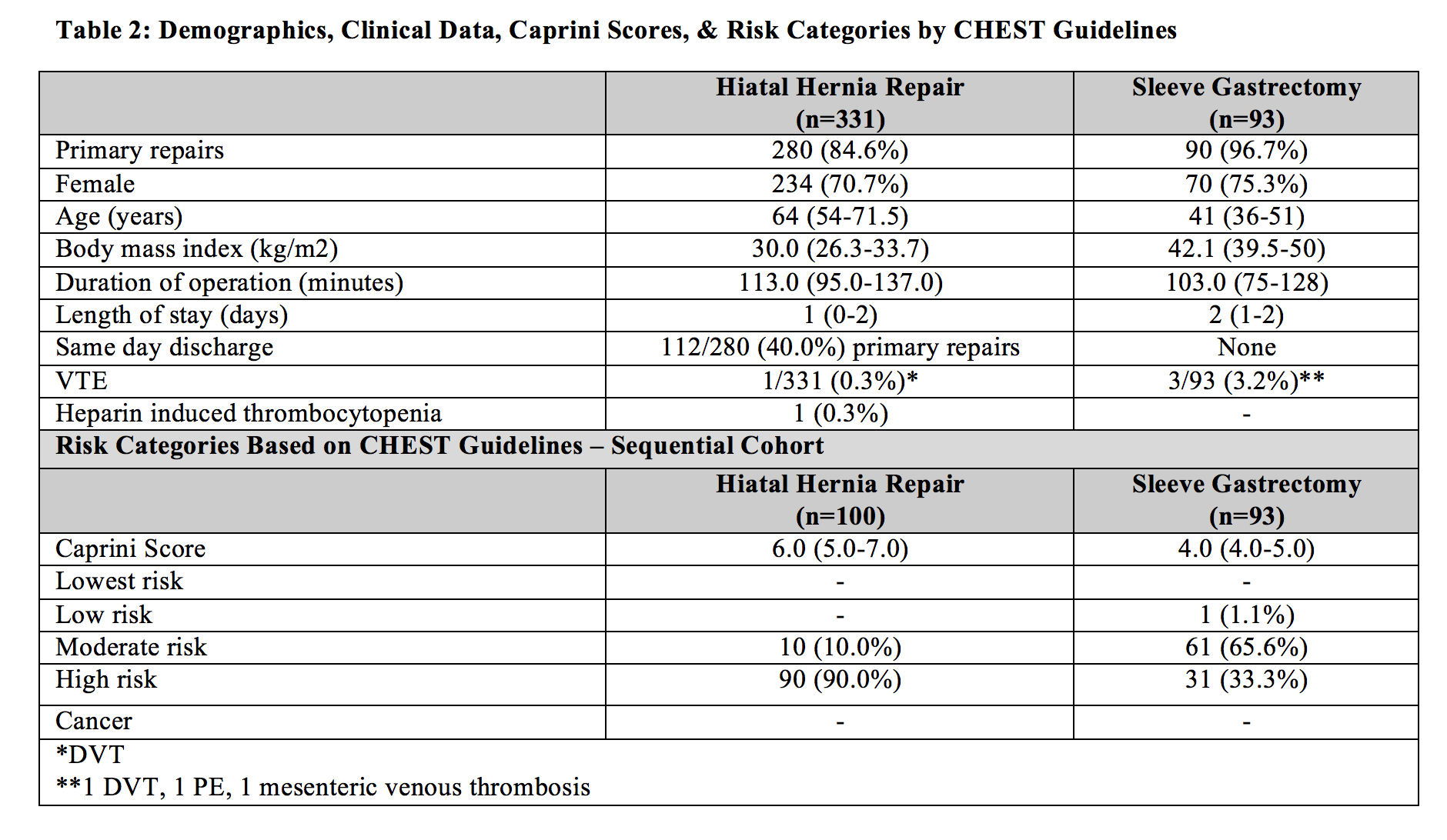
Table 2
Back to 2022 Posters
