THE TRUE EFFECT OF RACE: EFFECT MODIFICATION OF THE ASSOCIATION BETWEEN RACE AND MULTIMODAL THERAPY COMPLETION FOR PANCREATIC CANCER
Susanna W. de Geus*1, Marianna V. Papageorge1, Alison P. Woods1,2,3, Sing Chau Ng1, David Mcaneny1, Jennifer F. Tseng1, Teviah Sachs1
1Surgery, Boston Medical Center, Boston, MA; 2Beth Israel Deaconess Medical Center, Boston, MA; 3Johns Hopkins University, Baltimore, MD
Background: Socioeconomic status is a critical effect modifier in the association between race and treatment allocation. Race and socioeconomic status are often included in the same regression model and interpreted as a general measure of health inequality. However, these analyses do not elucidate the true effect of race. The present study investigates the association between race and receipt of multimodal therapy stratified by income and hospital volume.
Methods: Black and non-Hispanic White patients with clinical stage I and IIa pancreatic adenocarcinoma were identified from the National Cancer Database (2012-2016). Household income was estimated based on the patient's area of residence. Four separate cohorts were created: low-income patients treated at low-volume hospitals (LI-LV), high-income patients treated at low-volume hospitals (HI-LV), low-income patients treated at high-volume hospitals (LI-HV), and high-income patients treated at high-volume hospitals (HI-HV). In each cohort, multivariate logistic regression was performed to assess the impact of race on the likelihood of not undergoing pancreatic surgery and failure to receive multimodal therapy (surgery and chemotherapy), controlling for age, sex, comorbidities, stage, insurance status, and location.
Results: In total, 18,213 patients were identified; 4,254 patients in the LI-LV cohort (20.7%Black race), 5,866 patients in the HI-LV cohort (7.9% Black race), 3,297 patients in the LI-HV cohort (19.8% Black race), and 4,796 patients in the HI-HV cohort (7.1% Black race). On multivariate analysis, Black race did not significantly impact the likelihood of not undergoing pancreatic surgery for patients in the LI-LV (vs. White: OR, 1.09; p=0.340) or HI-LV cohort (vs. White: OR, 1.12; p=0.321). However, Black race was predictive for the likelihood of not undergoing pancreatic surgery among patients in the LI-HV (vs. White: OR, 1.49; p<0.001) and HI-HV cohort (vs. White: OR, 1.74; p<0.001). In addition, Black race was not predictive for failure to receive multimodal therapy among patients in the LI-LV (vs. White: OR, 1.10; p=0.593), HI-LV (vs. White: 0.98; p=0.910), or LI-HV group (vs. White: OR, 0.77; p=0.134), but did significantly impact the likelihood of not undergoing multimodal therapy among patients in the HI-HV cohort (vs. White: OR, 1.96; p=0.002).
Conclusions: Although patients treated at low-volume hospitals are generally less likely to receive multimodal therapy for pancreatic cancer, there is no difference between Black and White race patients at low-volume hospitals. However, among high-income patients at high-volume hospitals, Black patients are significantly less likely to receive multimodal therapy compared to White patients, even after controlling for confounding. These findings warrant further study of potential unconscious biases of patients and providers.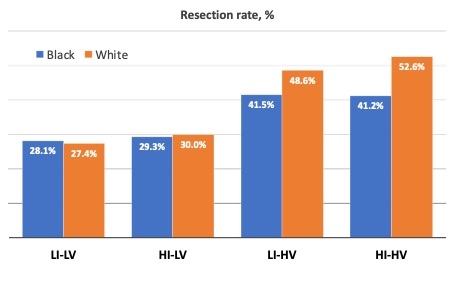
Figure 1. Resection rates of early-stage pancreatic cancer for Black and White race patients, stratified by income and hospital volume: low-income patients treated at low-volume hospitals (LI-LV), high-income patients treated at low-volume hospitals (HI-LV), low-income patients treated at high-volume hospitals (LI-HV), and high-income patients treated at high-volume hospitals (HI-HV).
Back to 2022 Abstracts
