BARIATRIC SURGERY IS ASSOCIATED WITH DECREASED UPPER GI BLEEDING IN HOSPITALIZATIONS FOR CIRRHOSIS: A NATIONWIDE STUDY
Vibhu Chittajallu*1, Yazan Abu Omar2, Miguel Salazar1, Roberto Simons-Linares2
1Digestive Health Institute, University Hospitals, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH
Background: Obesity is associated with non-alcoholic fatty liver disease which is now the leading cause of progression into cirrhosis. We investigate the inpatient clinical outcomes in obese patients hospitalized with decompensated cirrhosis and compare patients with history of bariatric surgery versus none.
Methods: We performed a case control study with the 2016 and 2017 National Inpatient Sample (NIS) using ICD10-CM and PCS codes to identify patients with obesity hospitalized with cirrhosis and those with history of bariatric surgery. Primary outcomes was mortality. Secondary outcomes were organ failures: acute kidney injury (AKI), respiratory failure requiring mechanical ventilation (MV), shock, sepsis, and length of stay (LOS). Multivariate regression models were constructed to adjust for confounders and hospital characteristics.
Results: A total of 63,550 (weighted) hospitalizations were included; 1,915 of which had a history bariatric surgery. More white patients were identified with cirrhosis after bariatric surgery (77.6% vs 68.2%, p = 0.00), while more Hispanic patients with cirrhosis without surgery (13.9% vs 8.6%, p = 0.00). More males without surgery were noted compared to with bariatric surgery (50.5% vs 25.5%, p = 0.00). In regards to comorbidities, bariatric surgery patients had lower rates of hypertension (55.4% vs 71.1%, p = 0.00) and diabetes mellitus (32.9% vs 53.7%, p = 0.00). There was no difference in mortality among groups. Bariatric surgery patients had lower rates of mechanical ventilation (1.6% vs 3.7%, p = 0.03), upper GI bleeding (4.2% vs 7.9%, p = 0.01), lower risk of inpatient upper GI bleeding (OR 0.51, 95% CI 0.31 – 0.84, p = 0.01). After adjusting for multiple comorbidities and baseline characteristics, bariatric surgery was still associated with decreased upper GI bleeding rates (adjusted OR 0.57, 95% CI 0.34 – 0.97, p = 0.04) and lower risk of inpatient mechanical ventilation (OR 0.41, 95% CI 0.18 – 0.93, p = 0.03).
Conclusion: History of bariatric surgery seems to be protective against inpatient upper GI bleeding and mechanical ventilation requirements for obese patients admitted for decompensated cirrhosis.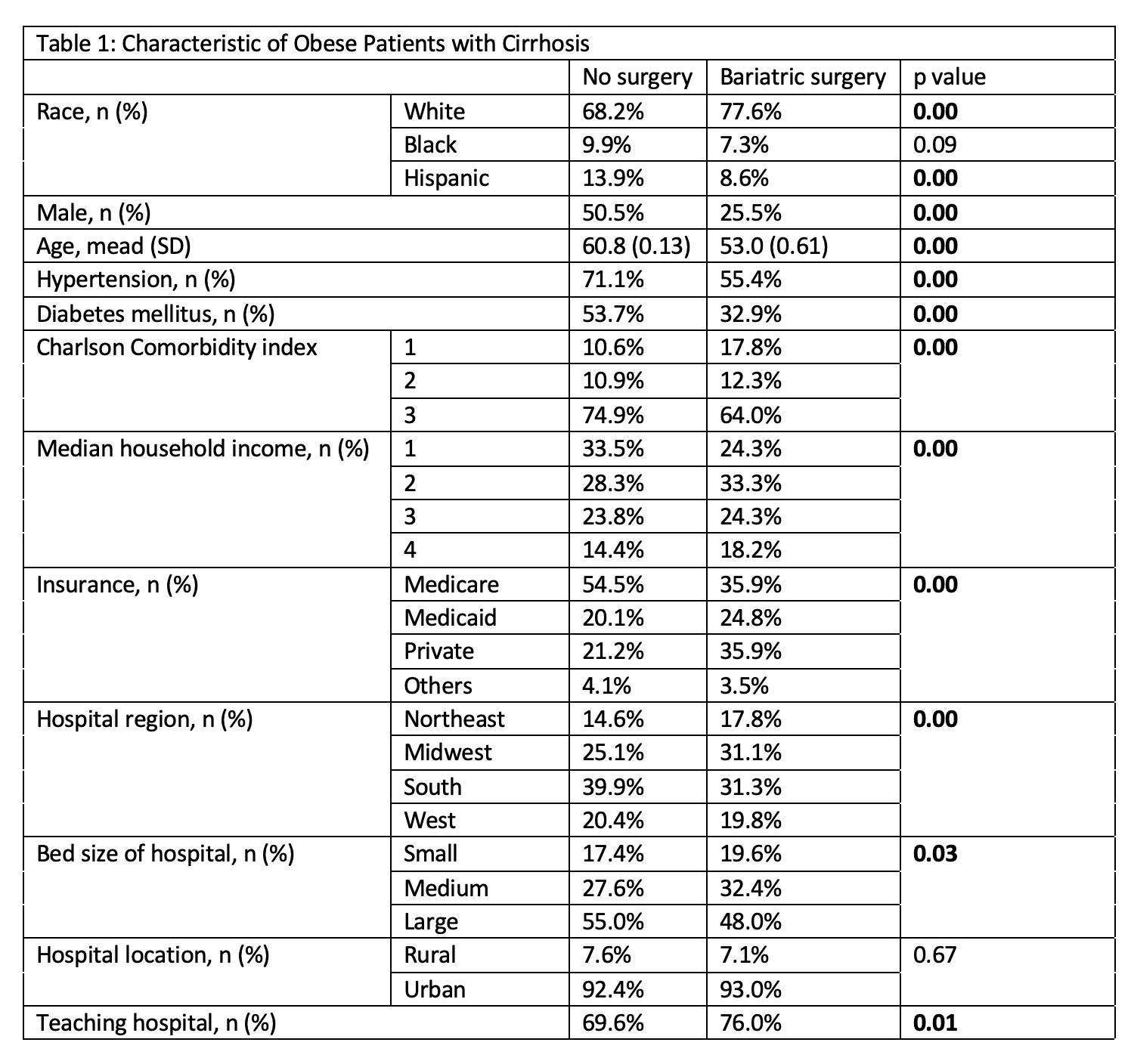
Table 1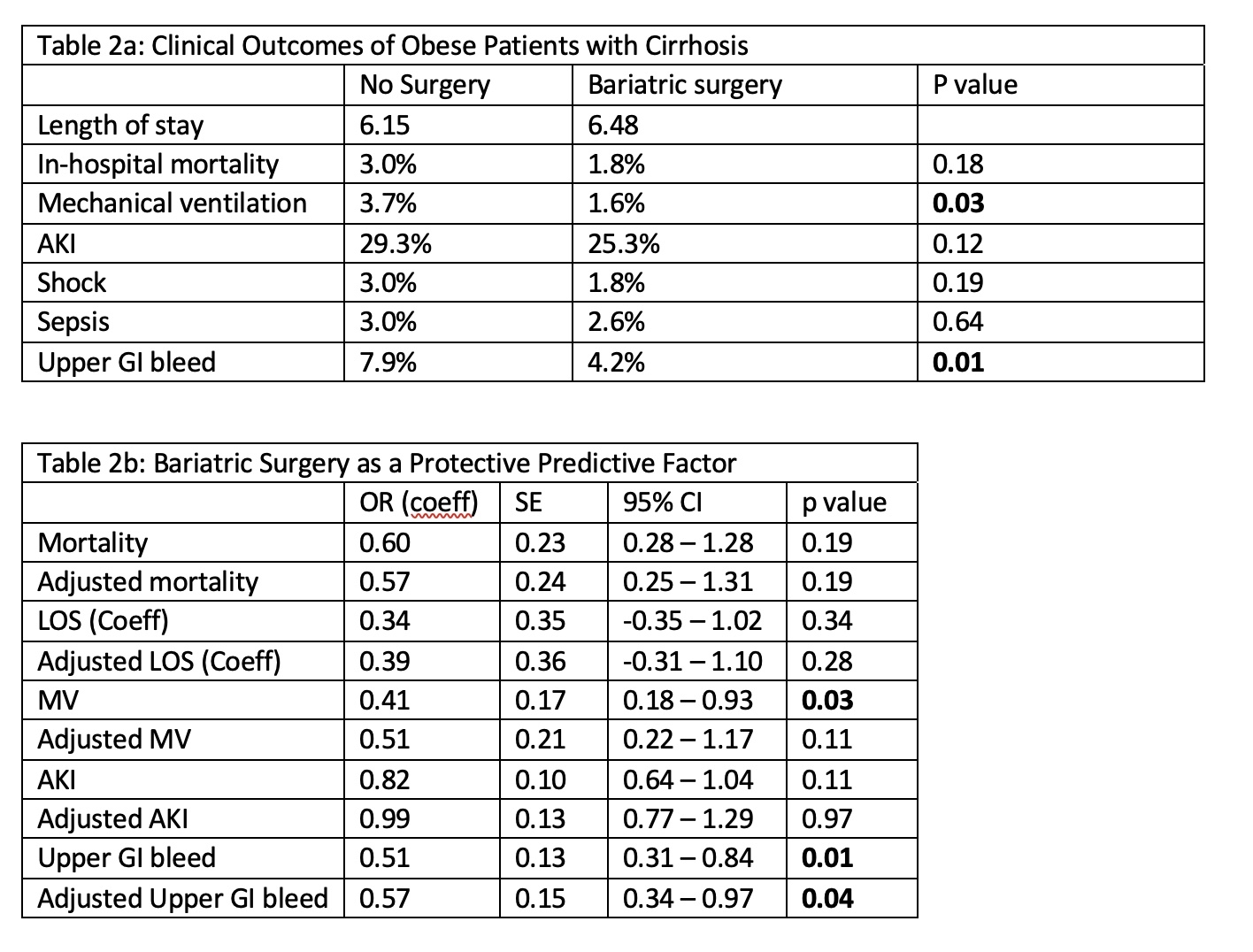
Table 2a/b
Back to 2022 Abstracts
