THE USE OF ANGIOTENSIN SYSTEM INHIBITOR IN THE SURVIVAL OF RESECTED PANCREATIC ADENOCARCINOMA PATIENTS
Hao Liu*1, Ibrahim Nassour1, Steven Lebowitz1, Mark D'Alesio1, Erica D. Hampton1, Annissa deSilva1, Abdulrahman Y. Hammad1, Samer AlMasri1, Hussein H. Khachfe1, Aatur Singhi1, Nathan Bahary2, Kenneth Lee1, Amer H. Zureikat1, Alessandro Paniccia1
1Surgery, UPMC, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA
Background
The Renin-angiotensin system (RAS) has crucial implications in pancreatic adenocarcinoma (PDAC) tumorigenesis and progression. Activities and inhibition of RAS may affect treatment response and may correlate with clinical outcomes. Previous observational studies suggested that angiotensin system inhibitor (ASI) use is associated with better survival in a subset of patients. Our present retrospective study focused on resected PDAC patients and explored the protective association of ASI.
Methods
A single-institution retrospective analysis of resected PDAC patients between 2010-2019. Clinicopathological characteristics of all cases meeting inclusion criteria were reviewed. To estimate the effect of ASI on patient survivals, we performed Kaplan Meier analysis, Cox Proportional Hazards model, Propensity Score Matching (PSM), and inverse propensity score weight (IPW) analysis. The propensity score of ASI treatment was calculated by comorbidities and treatments received.
Results
742 patients were included in the analysis. The average age is 67.0 (34 - 91) years old, with a median follow-up of 24.1 (3 - 122) months. ASI users are older (68.9 vs. 65.3, p<0.001) and with more comorbidities. Multivariate adjustment included clinicopathological parameters, comorbidities, and their treatments. The use of ASI is associated with significantly longer overall survival in univariate (HR=0.76[0.67-0.86], p=0.004) and multivariate (HR=0.71[0.57-0.89], p=0.003) adjusted analysis. In propensity score-matched cohort of 422 patients, ASI use is again associated with longer overall survival (HR=0.74[0.58-0.94], p=0.014) and a longer interval to disease progression in the liver and lung, but not local recurrence. Lastly, inverse probability weighting (IPW) analysis on the whole cohort of 742 patients suggested that the use of ASI is associated with an average treatment effect on the treated (ATT) of HR=0.67[0.53-0.85] (p<0.001) for overall survival.
Conclusion
In this single-institution retrospective study focusing on resected PDAC patients, the use of ASI is associated with longer overall survival after adjusting for multiple clinicopathological parameters. Propensity score matching and IPW analysis also showed that ASI use is associated with longer overall and progression-free survival. Further prospective trial on resectable PDAC is needed.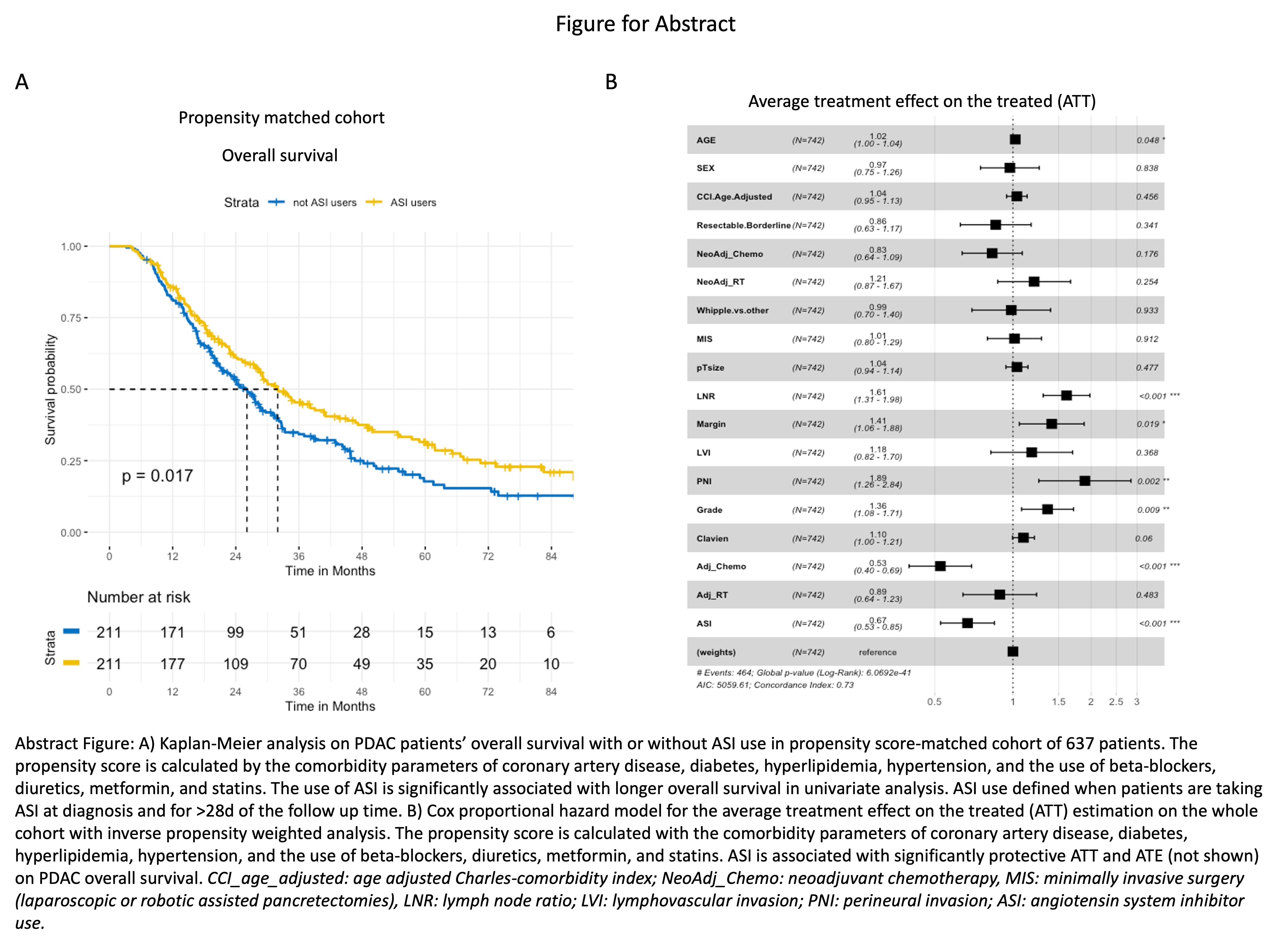
Abstract Figure: A) Kaplan-Meier analysis on PDAC patients' overall survival with or without ASI use in propensity score-matched cohort of 637 patients. The propensity score is calculated by the comorbidity parameters of coronary artery disease, diabetes, hyperlipidemia, hypertension, and the use of beta-blockers, diuretics, metformin, and statins. The use of ASI is significantly associated with longer overall survival in univariate analysis. ASI use defined when patients are taking ASI at diagnosis and for >28d of the follow up time. B) Cox proportional hazard model for the average treatment effect on the treated (ATT) estimation on the whole cohort with inverse propensity weighted analysis. The propensity score is calculated with the comorbidity parameters of coronary artery disease, diabetes, hyperlipidemia, hypertension, and the use of beta-blockers, diuretics, metformin, and statins. ASI is associated with significantly protective ATT and ATE (not shown) on PDAC overall survival.
Back to 2022 Abstracts
