IMPROVEMENT IN OPERATIVE TIMES WITH COOPERATIVE PANCREATICODUODENECTOMY AT AN ACADEMIC COMMUNITY CANCER CENTER
Yarrow Sheldon*, Bormann Bradford, Raafat Abdel-Misih, Nicholas Petrelli, Gregory Tiesi
Surgical Oncology, Christiana Care Health Services Inc, Wilmington, DE
Introduction
Pancreaticoduodenectomy (PD) is a complex surgical procedure with high risk for morbidity and mortality. While many publications have examined the impact of volume on outcomes, few have examined the impact of cooperative surgery with 2 trained surgical oncologists. In 2015, our institution started to transition to combined PD (CPD) with 2 fellowship trained surgical oncologist to optimize OR efficiency, and by extension, outcomes. Here, we present our experience.
Methods
A retrospective review was performed for all patients at our academic community center who underwent a CPD between January 2015 to November 2021. The primary outcome was operative time. The secondary outcomes were 30-day mortality, re-laparotomy, re-admission, length of inpatient stay (LOS), estimated blood loss (EBL), transfusion requirement, major Clavien-Dindo (CD) complications (?III), delayed gastric emptying (DGE), pancreatic fistula (all grades), surgical site infection, hemorrhage (requiring ?4U or intervention), pneumonia (PNA), venous thromboembolic event (VTE), anastomotic leak, sepsis, or acute renal failure. Patients were excluded if they had additional procedures at the time of their CPD. 2019 was used as a cutoff as 70% or more of the yearly PD were CPD. Analyses were performed using Unpaired T-tests and Fisher's exact tests.
Results
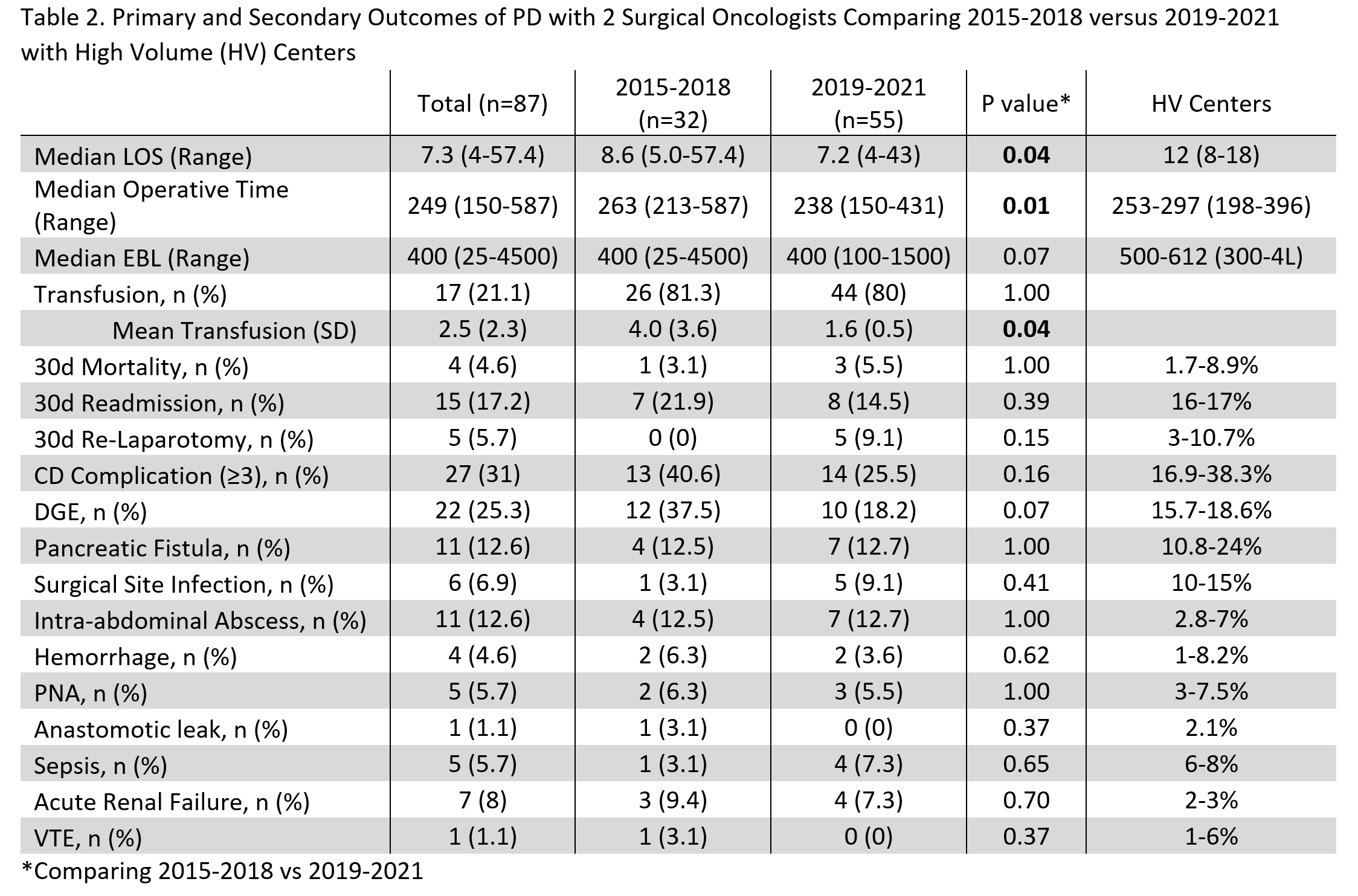
After exclusion criteria, 87 CPD patients were identified (Table 1). The average age was 69.2 ±11.1. 44.8% were male. The average BMI was 28.9 ± 5.9. 13 ± 7.5 CPD were performed per year, starting with 3 in 2015 increasing to 24 in 2020. The median operative time was 249 (150-587) minutes with an EBL of 400 (25-4500) mL (Table 2). Only 17 (21.1%) cases required intra-operative transfusion with an average transfusion of 2.5 ±2.3 units. The median LOS was 7.3 (4-57.4) days.
Overall, 30-day mortality was 4.6%. 15 (17.2%) patients had 30-day readmission. 5 (5.7%) had 30-day re-laparotomy. There were 14 (16.1%) grade III and 9 (10.3%) grade IV CD complications. 22 (25.3%) patients had DGE, 8 (9.2%) required gastrojejunostomy tube placement, 11 (12.6%) pancreatic fistulas, and 11 (12.6%) intra-abdominal abscesses.
In 2015-2018 vs 2019-2021, the LOS (8.6 vs 7.2d), operative time (263 vs 238min), and transfusions (4 vs 1.6U) were statistically improved with the increased rate of CPD. The major complication rate (40.6% vs 25.5%) and DGE (37.5% to 18.2%) were nearly halved, but the re-laparotomy rate increased with time (0 vs 9.1%). Our data from 2019-2021 compared favorably to published data from high volume (HV) centers, especially the median operative time.
Conclusion
Transition to CPD at our community cancer center led to significantly shorter operative times and decreased length of stay. These, as well as many of our secondary outcomes, compared favorably to other HV centers. Adoption of CPD at may offset the procedure's known risks.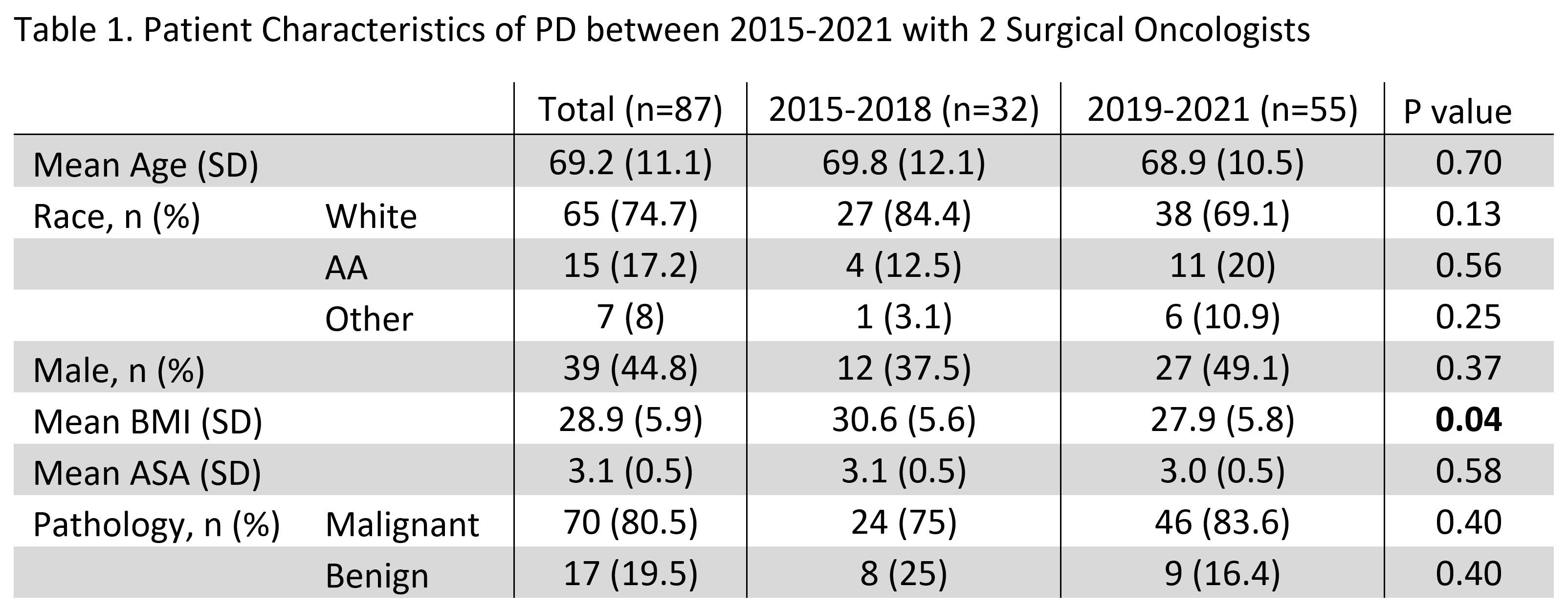
Back to 2022 Abstracts
