PREOPERATIVE FACTORS IMPACT ON POSTOPERATIVE BLOATING
Rodrigo C. Edelmuth*1,2, Federico Palacardo1, Jacques A. Greenberg1, Caitlin Egan1, Yeon Joo Lee1, Maria Cristina Riascos1, Murtaza Qazi1, Felice Schnoll-Sussman1, Philip O. Katz1, Brendan M. Finnerty1, Thomas J. Fahey1, Rasa Zarnegar1
1Surgery, Weill Cornell Medicine, New York, NY; 2Hospital Israelita Albert Einstein, Sao Paulo, São Paulo, Brazil
Introduction: Bloating is one of the dreaded side effects of anti-reflux surgery (ARS) leading patients and clinicians to offer alternative treatments. However, there is limited data to determine the incidence of new onset bloating post ARS. We aimed to evaluate the effect of ARS on postoperative bloating and to determine factors that could be related to preoperative and postoperative bloating.
Methods: A prospectively database of patients undergoing robotic ARS between January 2012 and October 2021 was reviewed for demographic and perioperative details. Inclusion criteria was patients undergoing index ARS without a combined procedure. Patients with previous foregut surgery were excluded. Perioperative characteristics were compared across two groups dependent upon the presence of bloating. An online survey containing a modified version of the seven-item severity in general (SevGen) from the Bloating Severity Questionnaire (BSQ) was sent to all patients. Bloating characteristics were compared before and after ARS. Wilcoxon signed-rank tests and Chi-Square tests were used to compare continuous and categorical variables where applicable, respectively.
Results: There were 428 patients that met inclusion criteria, of which 104 (24.3%) complained of preoperative bloating. Most patients were female (61%), mean age was 53.4 and mean BMI was 25.3. Preoperative characteristics were similar between groups with no statistical significance. Preoperative tests results, including manometry findings, BRAVO, esophagram and upper endoscopy did not seem to be related to preoperative bloating sensation. Preoperative Barrett's esophagus was only found in patients who had postoperative bloating (20.4%, p=0.02). The median time from surgery to BSQ completion was 27 months (IQR 8 - 56). Of the 428 patients, 94 completed the BSQ post-operatively. Most patients reported experiencing abdominal bloating before and after ARS (55.3% vs. 57.5, p=0.8). However, new or worsening bloating sensation was seen in 23.4%. New onset of bloating developed only in 2 patients (3.7%). Nissen fundoplication had a significant higher rate of new/worsening bloating if compared to Toupet, Hill and Linx (68%, 23%, 9%, 0; p=0.04), respectively. Although not statistically significant, bloating severity and monthly frequency tended to be lower after surgery (1.6 ± 1.7 vs. 1.3 ± 1.4, p=0.42; 10 days ± 12 vs. 7 days ± 10, p=0.26). Patients who never reported pain along with the bloating increased (27% to 39%, p=0.1) and its severity decreased (4.3 ± 2.9 to 3.5 ± 2.9, p=0.13). Daily discomfort other than pain along with the bloating also decreased (42.3% vs. 14.8%, p < 0.02).
Conclusions: New or worsening bloating occurs in 23% of patients post ARS with Nissen fundoplication causing the majority. Tailored surgery specially in the presence of preoperative bloating may be warranted.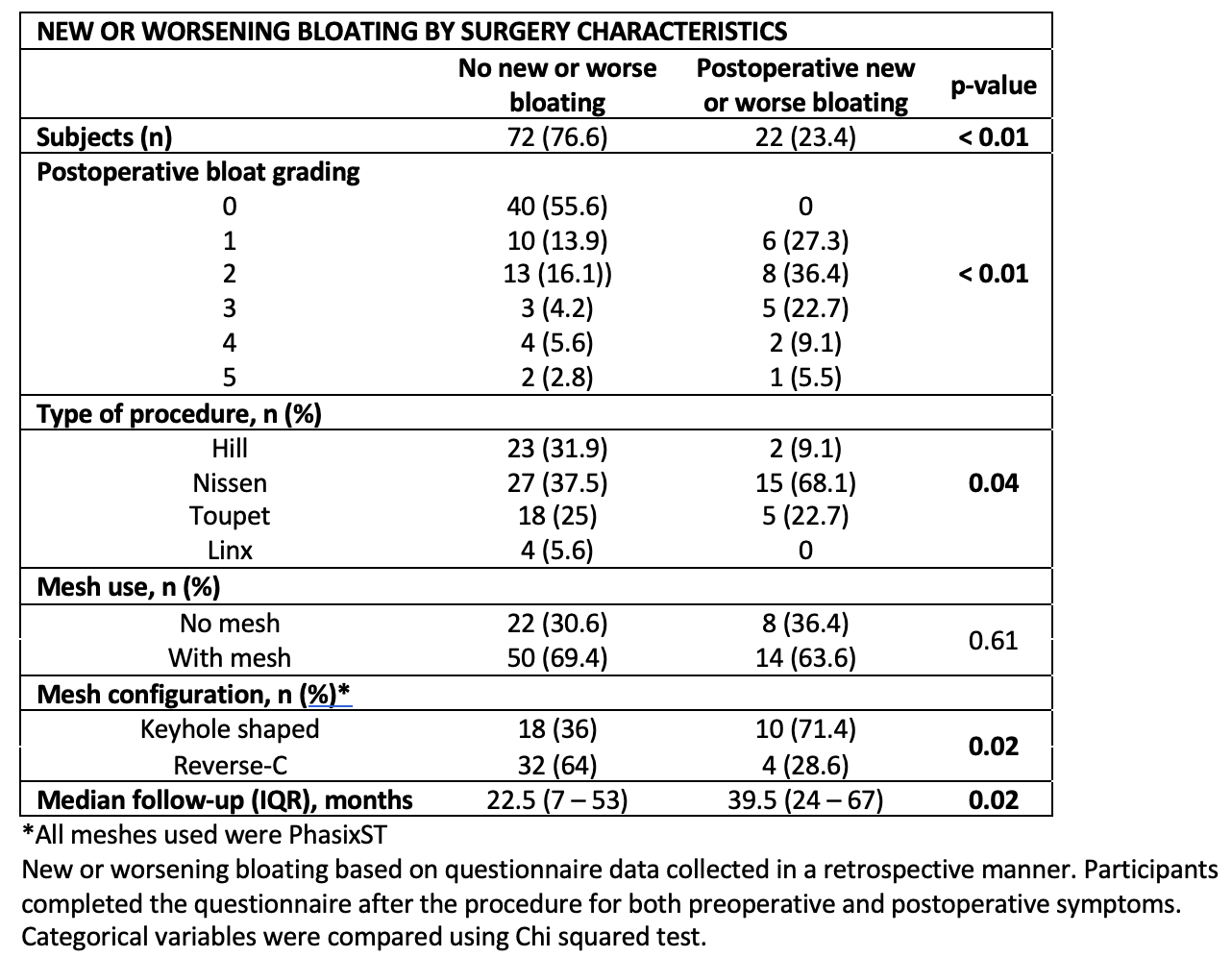
POSTOPERATIVE BLOATING BY SURGERY CHARACTERISTICS 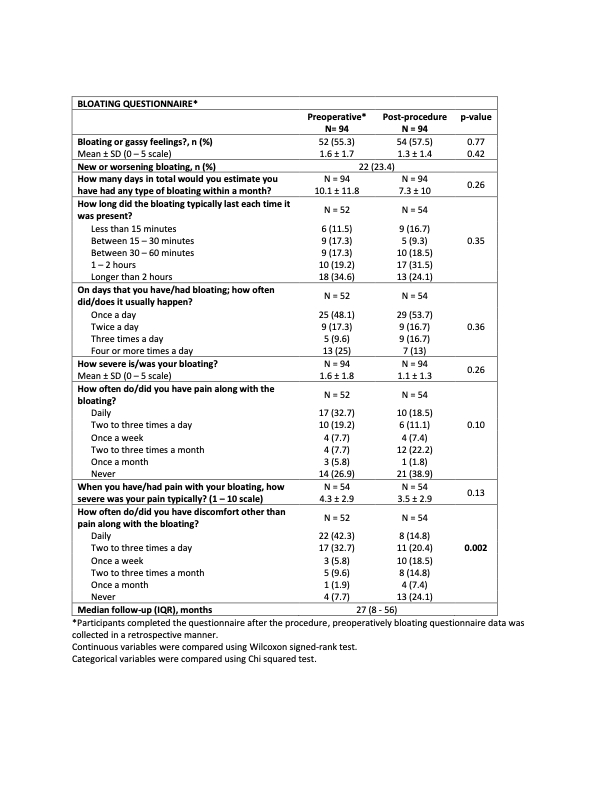
BLOATING QUESTIONNAIRE
Back to 2022 Abstracts
