OBESITY AND HIATAL HERNIA REPAIRS, IS IT TIME TO ESTABLISH A NEW PARADIGM?
Shankar Logarajah*1, David Ahle1, Muhammad B. Darwish3, Maitham A. Moslim1, Michael Jureller1, Houssam Osman1,2, D. Rohan Jeyarajah1,2
1Methodist Richardson Medical Center, Richardson, TX; 2Texas Christian University, Fort Worth, TX; 3Valley Health System, Las Vegas, NV
Introduction
Hiatal Hernia repairs are increasingly performed operations in the United States. While the methodology of repairing a hiatal hernia has become a well established the recurrence rate after these procedures has historically been reported to be as high as 14-25%. Obesity has long been established as a predictor of repair failure owing to increased intra-abdominal pressure. We seek to test whether this holds true in the era of improved surgical technology and whether there are any patient characteristics that are associated with a higher rate of failure.
Methods and Procedures
A retrospective chart review of patients who were underwent hiatal hernia repair at a single surgical practice was conducted. Patients were stratified into groups regarding whether they had a previous hiatal hernia repair at time of surgery or not. Univariate analysis was performed between groups to test significant patient demographic factors and clinical symptoms. A p value less than 0.05 was considered significant.
Results
64 patients were identified who underwent hiatal hernia repair between 2014 and 2020. 44 (68.7%) underwent repair for the first time while 20 (31.2%) underwent a repair for a second or greater time. Gender (p = 0.849) and comorbidities such as hypertension (p = 0.781), diabetes (p = 0.884), and dyslipidemia (p = 0.683) did not differ significant between groups. Weight loss and dysphagia was found to be present in of patients with a prior repair more frequently (33.3% vs 7.3%, p = 0.041) (70% vs 38.6%, p = 0.02). Other symptoms such as symptomatic anemia (p = 0.533) and chest pain (p = 0.227) were not found to be significant different. Lastly, BMI was found to be significantly higher in patients requiring re-operative repair (36.1 kg/m2 vs 30.7 kg/m2, p = 0.018).
Conclusion
Obesity has long been associated with hiatal hernia repair failure. Current standard of care have not been established for alternative procedures instead of a traditional repair to be performed. We observe that patients requiring re-operative hiatal hernia repairs have a significantly increased BMI and are more symptomatic. Select groups have published promising data regarding roux-en-y gastric bypass as a possible way to reduce hiatal hernia recurrence in obese patients and future studies should aim to validate this procedure for this patient population further.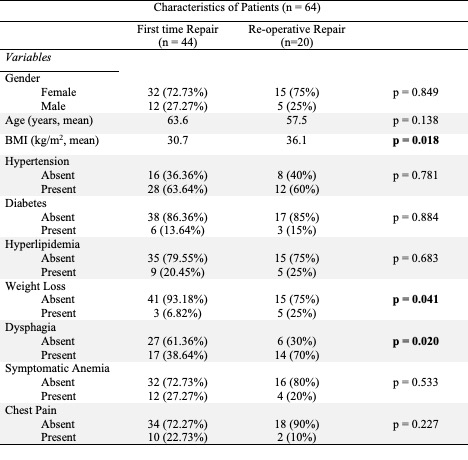
Back to 2022 Posters
