USING AN ENDOLUMINAL FUNCTIONAL LUMEN IMAGING PROBE (ENDOFLIP) TO COMPARE PYLORIC FUNCTION IN PATIENTS WITH GASTROPARESIS TO PATIENTS AFTER ESOPHAGECTOMY
Florian Lorenz*1, Stefanie brunner1, Felix Berlth2, Ulrich Toex1, Isabel Rieck1, Lea Streller1, Peter P. Grimminger2, Christiane J. Bruns1, Tobias Goeser1, Seung-Hun Chon1
1Uniklinik Koln, Koln, Nordrhein-Westfalen, Germany; 2Universitatsmedizin der Johannes Gutenberg-Universitat Mainz, Mainz, Rheinland-Pfalz, Germany
Objective for the study
Delayed gastric emptying (DGE) occurs in patients suffering from gastroparesis caused by, e.g., diabetes mellitus or systemic sclerosis, as well as in patients after esophagectomy. DGE causes a significant reduction of quality of life due to nausea and vomiting. Pyloric dysfunction is considered one of the main mechanisms that cause DGE and, therefore, a potential therapeutic target. To get a better understanding of the pathophysiology of DGE, our study measured pyloric distensibility using EndoFlipTM and compared pyloric function in post-surgical as well as in non-surgical gastroparesis patients.
Methods and procedures
This retrospective study took place at a national referral center for tumor entities of the upper gastrointestinal tract, and the data was collected from the hospital's patient database. In total, 83 Patients underwent a measurement of the pylorus with the EndoFlipTM. Twelve patients who suffered from gastroparesis due to diabetes mellitus, systemic sclerosis or idiopathic causes were compared to 28 patients who received an esophagectomy and suffered from delayed gastric conduit emptying (DGCE) and to a further 43 patients who were asymptomatic after esophagectomy between 01/03/2021 and 30/11/2021. An esophagogastroduodenoscopy under sedation was performed in all patients, and the EndoFlipTM was positioned under endoscopic control. Distensibility was measured at 40ml, 45ml and 50ml balloon filling. The statistical analysis was performed using SPSS. The Student t-test and Chi Square test were used. All tests were two-sided, with statistical significance set at p ? 0.05.
Results
The EndoFlipTM measurement was feasible in all patients, and no complications were recorded. Distensibility proved to be similar in patients suffering from gastroparesis and DGCE. Comparing those groups to asymptomatic post-esophagectomy patients, pyloric distensibility was overall smaller than in asymptomatic patients. At 40ml, 45ml and 50ml balloon filling, the mean distensibility in gastroparetic patients was 8.7, 6.1 and 4.8 mm2/mmHg. In post-surgical patients suffering of DGCE, the distensibility was 6.3, 5.4 and 4.6 mm2/mmHg. In asymptomatic post-surgical patients, the distensibility was 9.8, 7.6 and 5.6 mm2/mmHg. Differences between symptomatic and asymptomatic patients were significant.
Conclusion
Pyloric dysfunction is a common pathomechanism in patients suffering from gastroparesis and DGCE. Asymptomatic post-esophagectomy patients seem to have a higher pyloric distensibility, despite having a disrupted vagal nerve post-surgery. Pyloric distensibility and symptoms of DGE or DGCE seem to correspond. Thus, we may use pyloric distensibility as a possible new marker to better identify patients suffering of pyloric dysfunction and to introduce them to adequate therapy, such as, pneumatic dilation or pylorus myotomy.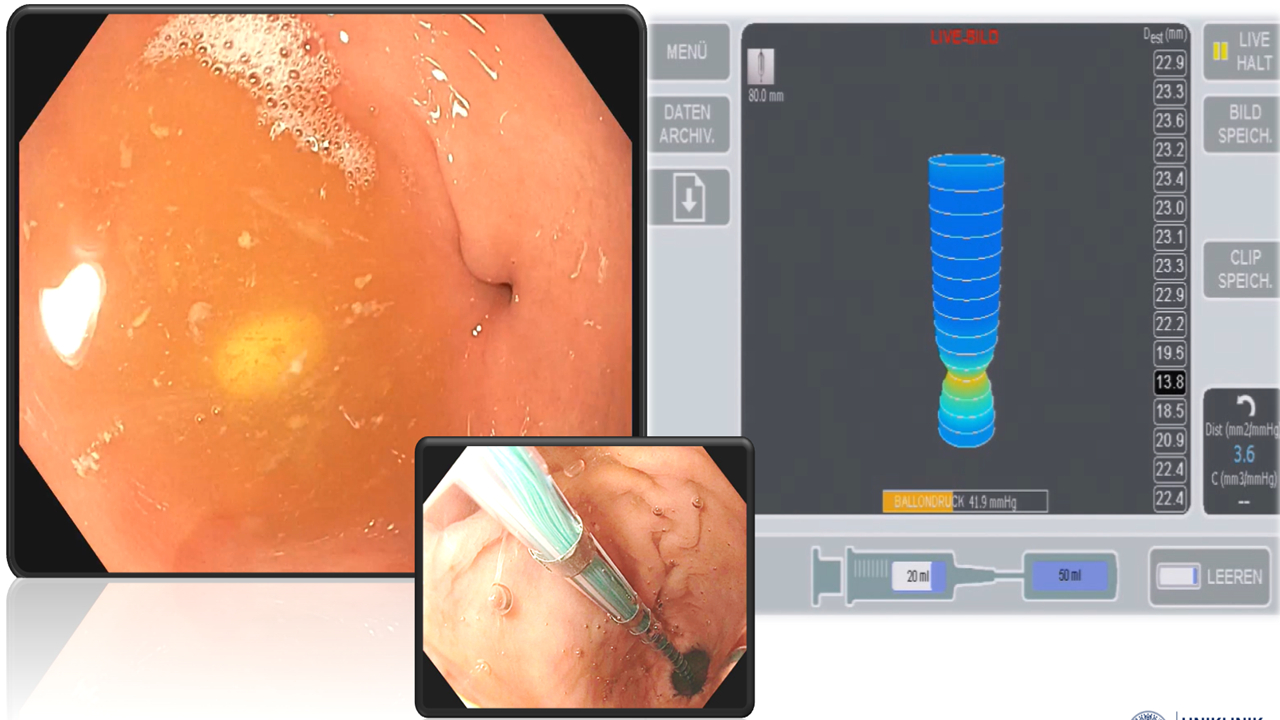
Delayed gastric conduit emptying (DGCE) after esophagectomy
Left: Pylorus endoscopically
Middle: Measurement of the pylorus with the endoflip-katheter
Right: Distensibility of the pylorus
Back to 2022 Abstracts
