ESOPHAGEAL MOTILITY PATTERNS IN PARAESOPHAGEAL HIATUS HERNIA
Rocio Carrera Ceron*, Robert B. Yates, Andrew S. Wright, Brant K. Oelschlager, Roger P. Tatum
Department of Surgery, University of Washington, Seattle, WA
Objective: To describe the rates of esophageal motility disorders in patients with paraesophageal hiatus hernia (PEH).
Background: The use of high-resolution manometry (HRM) has led to an increase in the diagnosis of esophageal motor dysfunction. Esophageal motility disorders are common in patients referred for HRM; in particular, ineffective esophageal motility (IEM) is known to occur in up to 17% of otherwise healthy individuals. In patients with PEH, many of whom also have gastroesophageal reflux disease (GERD), the anatomic course of the esophagus is altered significantly, which may be more likely to result in motility abnormalities. Clinical implications of this relationship have to do with symptom presentation and severity, and decision making prior to surgery.
Methods: All patients referred for high-resolution manometry (HRM) to a tertiary care university hospital between 2015 and 2019 were included in a prospectively maintained database. HRM studies were analyzed for the appearance of any esophageal motility disorder and the relative rates of each were determined.
Results: Of 3649 patients undergoing HRM between 2015 and 2019, 332 had a diagnosis of PEH later confirmed at operation. Rates of any motility disorder in PEH were 42%. Specific disorders included IEM in 32.6%, esophagogastric junction (EGJ) outflow obstruction (by manometric criteria) in 8%, distal esophageal spasm in 0.6%, hypercontractile esophagus in 0.4%, and absent contractility in 0.4%. There were no patients with achalasia (Table).
Conclusions: Overall, motility disorders were common in PEH patients, with higher rates of IEM and manometric EGJ outflow obstruction than seen in the general population. This may represent physiologic sequelae of the anatomic derangement of the distal esophagus due to the presence of the hiatus hernia, and potentially has implications in the options for surgical management of PEH. These findings suggest that HRM is still useful and necessary in the preoperative workup of PEH patients.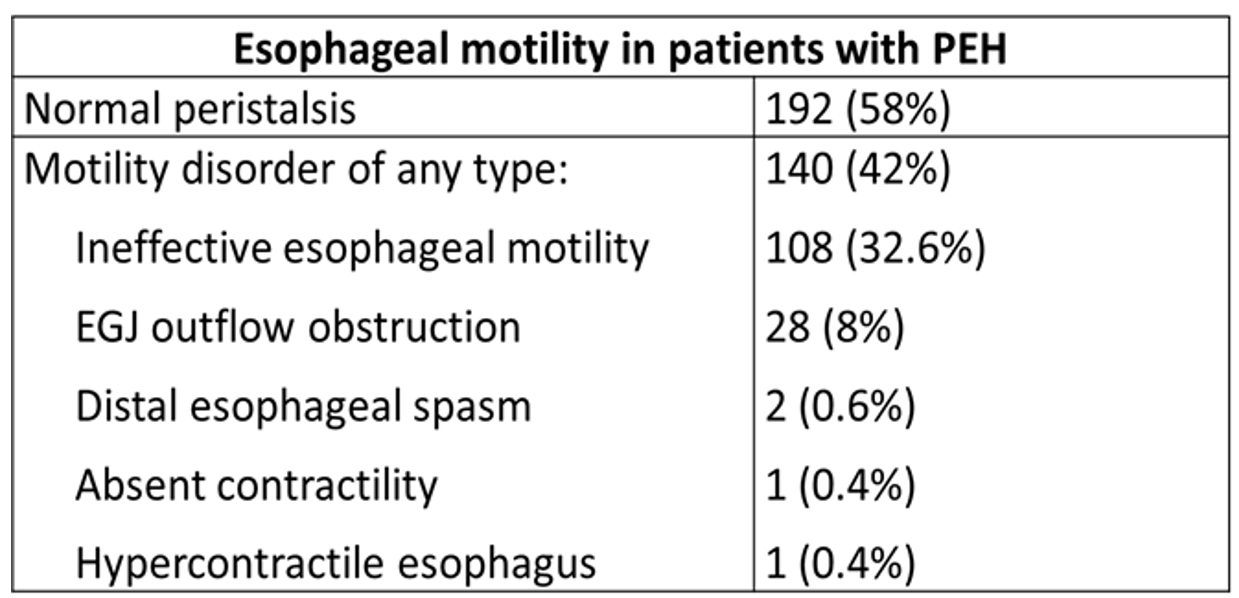
Back to 2022 Abstracts
