CLINICOPATHOLOGICAL IMPACT OF THE BORRMANN TYPE IN ADVANCED GASTRIC CANCER
Yuki Hirata*, Annamaria Agnes, Laura R. Prakash, Paul Mansfield, Brian Badgwell, Naruhiko Ikoma
The University of Texas, MD Anderson Cancer Center, Department of Surgical Oncology, Houston, TX
Background: Morphologic characteristics of gastric cancers are known to be associated with treatment response and survival outcome. Compared with gastric tumors with clear demarcation edges (Borrmann type 1/2), gastric tumors with diffuse and infiltrative tumor morphology (Borrmann type 3/4) have higher rates of positive-margin resection and peritoneal metastasis and are associated with significantly shorter survival outcome, based on reports from Asian countries. However, the association between morphologic characteristics and treatment outcome in gastric cancer remains unknown in Western countries. The purpose of this study was to determine the effect of Borrmann type on the rate of pathologic complete response after preoperative therapy in gastric cancer in the United States.
Methods: Patients with gastric cancer who received neoadjuvant therapy followed by curative-intent gastrectomy were identified from a prospectively maintained single-institutional database (January 2017 through October 2019). Patients who had pretreatment endoscopic images available for review in their electronic medical records were enrolled. Two surgeons independently reviewed pretreatment endoscopic pictures and classified tumors according to Borrmann type. Clinicopathological characteristics were summarized by Borrmann type and compared with use of chi-square tests. We investigated the association between Borrmann types and complete response rate by using a logistic regression model.
Results: Of the 146 patients who underwent gastrectomy during the study period, 49 with available pretreatment endoscopic images were enrolled in this study. We classified the tumors as follows: Borrmann type 1, 1 tumor (2%); type 2, 13 (26%); type 3, 23 (47%); and type 4, 12 (25%). The concordance rate of Borrmann type classification between surgeons was 92% (45/49). Borrmann type was not associated with poorly differentiated grade (type 1/2, 64%; type 3/4, 74%; p = 0.263) or signet ring cell histology (type 1/2, 57%; type 3/4, 51%; p = 0.717). Complete response rates were 36% (5/14) in type 1/2 and 6% (2/35) in type 3/4 tumors (p = 0.018). A multivariable logistic regression model showed that Borrmann type 3/4 was the only independent factor associated with reduced likelihood of complete response (odds ratio 0.14; p = 0.045). Overall survival was less in Borrmann type 3/4 than in type 1/2, although the difference was not statistically significant (p = 0.16) (Figure 1).
Conclusion: In this study, the patients received neoadjuvant therapy with Borrmann classification type 3/4 gastric cancer had a lower likelihood of achieving pathological complete response after preoperative therapy and appeared to have diminished survival after gastrectomy. A larger study to validate these findings is warranted to enable possible treatment stratification based on tumor morphology of gastric cancer.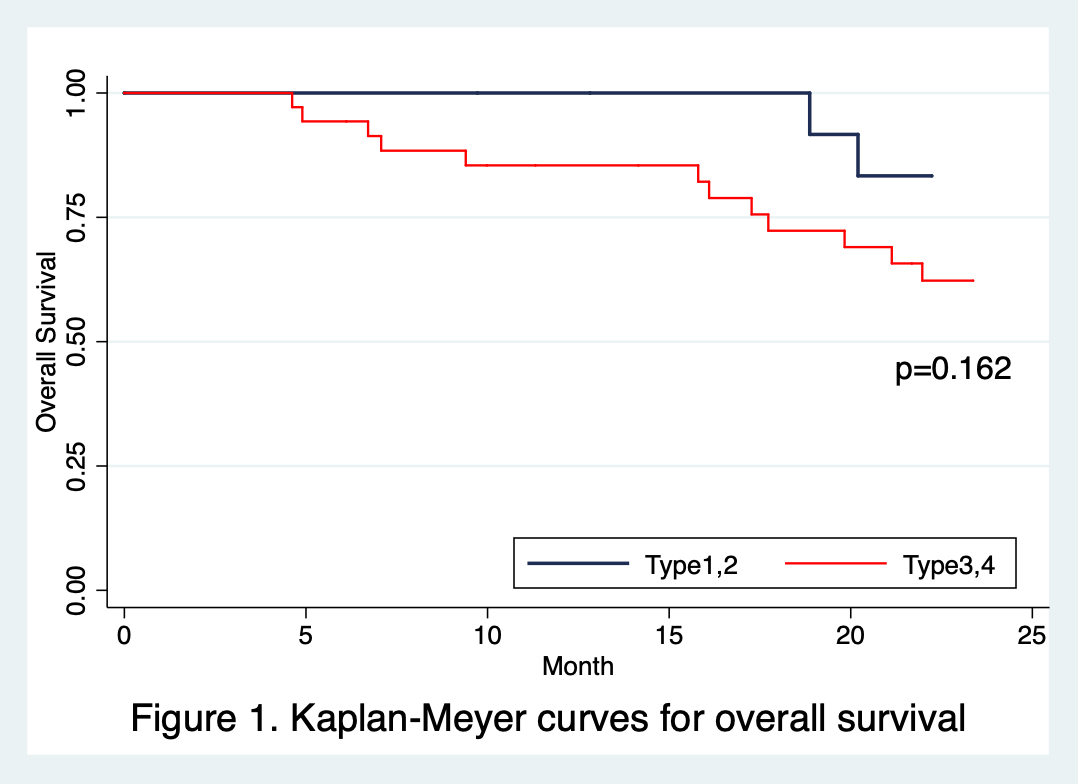
Back to 2022 Abstracts
