RECURRENCE RATES OF ADVANCED NEOPLASIA AFTER ENDOSCOPIC OR SURGICAL RESECTION IN INFLAMMATORY BOWEL DISEASE PATIENTS: A RETROSPECTIVE COHORT STUDY
Monica E. Derks*1, Maarten te Groen1, Charlotte P. Peters2, Gerard Dijkstra3, Annemarie C. De Vries4, Tessa Romkens5, Carmen S. Horjus Talabur Horje6, Nanne De Boer7, Iris D. Nagtegaal8, Lauranne Derikx1, Frank Hoentjen1,9
1Gastroenterology and Hepatology, Radboudumc, Nijmegen, Gelderland, Netherlands; 2Amsterdam UMC Locatie AMC, Amsterdam, North Holland, Netherlands; 3Universitair Medisch Centrum Groningen, Groningen, Groningen, Netherlands; 4Erasmus MC, Rotterdam, Zuid-Holland, Netherlands; 5Jeroen Bosch Ziekenhuis Afdeling Maag- Darm- en Leverziekten, 's-Hertogenbosch, Noord-Brabant, Netherlands; 6Rijnstate, Arnhem, Gelderland, Netherlands; 7Amsterdam UMC Locatie VUmc, Amsterdam, Noord-Holland, Netherlands; 8Radboudumc, Nijmegen, Gelderland, Netherlands; 9University of Alberta, Edmonton, AB, Canada
Background
Inflammatory bowel disease (IBD) patients are at increased risk of advanced neoplasia (AN) including high grade dysplasia (HGD) and colorectal cancer (CRC). Historically, a (sub)total colectomy was recommended in these patients, but alternatively, endoscopic resection or partial colectomy can be considered as well. We aimed (1) to identify factors associated with AN treatment choice and (2) to assess AN recurrence rates following different treatment modalities.
Methods
In this retrospective multi-center cohort study we used the Dutch nationwide histopathology registry (PALGA) to identify ulcerative colitis (UC), Crohn's disease (CD) and IBD-unclassified patients diagnosed with colonic AN between 1991 and 2020 in seven hospitals in the Netherlands. Exclusion criteria were familial CRC or AN prior to IBD diagnosis. Data regarding the first (index) AN, treatment and endoscopic and surgical follow-up were collected. Recurrence was defined as colorectal AN (independent of colonic location) detected after treatment of index AN. Multinomial logistic regression and cox regression analysis were used to assess in respective associations with treatment choice and recurrence free survival.
Results
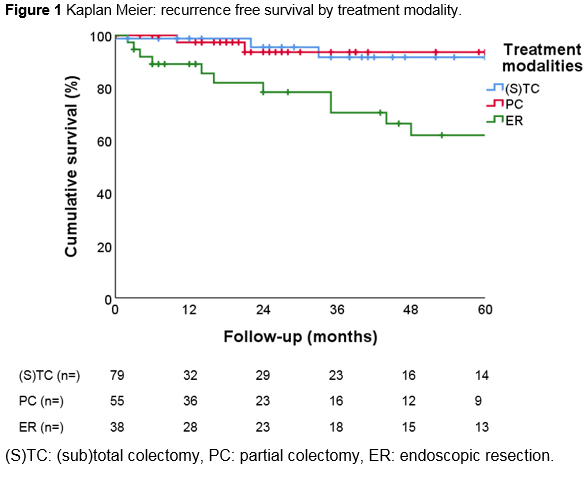
We included 189 patients with index AN (n=81 HGD, n=108 CRC) with a median follow up of 27 months (IQR 7-69 months). (Sub)total colectomy was performed in 79 patients (41.8%; n=33 HGD, n=46 CRC), whereas 55 patients (29.1%; n=12 HGD, n=43 CRC) had a partial colectomy. Endoscopic resection was performed in 38 patients (20.1%; n=35 HGD, n=3 CRC), of which EMR/ESD n=12 (6.3%). Seventeen lesions (8.9%; n=1 HGD, n=16 CRC) were not removed, due to comorbidity or metastatic disease. CRC, primary sclerosing cholangitis (PSC), extensive disease and younger age at time of index AN were associated with (sub)total colectomy (Table 1). Twenty-one patients (12.2%) developed recurrence AN (n=12 HGD, n=9 CRC), after a median of 24 months (IQR 14-48; figure 1). Endoscopic resection was associated with recurrence (adjusted hazard ratio 4.0, confidence interval [1.3-12.2], p=0.02), as 14/21 patients (66.7%) with recurrence were initially (for index AN) treated with endoscopic resection. In addition, 3 patients (14.3%) were treated with partial colectomy and 4 (19.0%) with (sub)total colectomy. In 11/21 patients (52.4%) recurrence was treated with surgical resection.
Conclusions
Factors associated with AN treatment with (sub)total colectomy were CRC, PSC, extensive disease and younger age. After AN treatment, 1 out of 10 IBD patients developed recurrence of AN, mainly after endoscopic resection. This underlines the importance of stringent endoscopic surveillance following treatment of AN, especially after endoscopic resection with residual colon in place.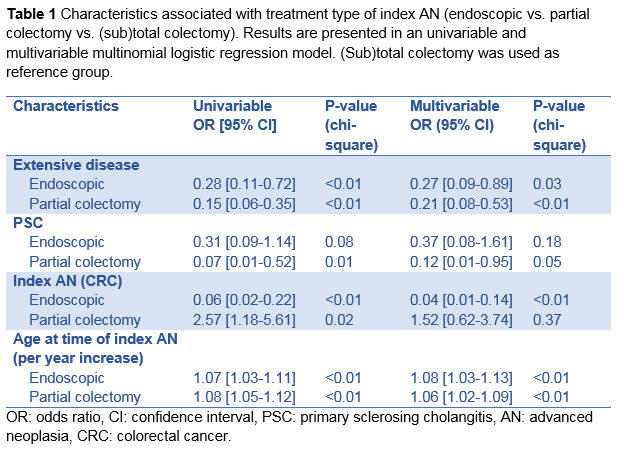
Back to 2022 Abstracts
