STAGING ENDOSCOPIC FULL THICKNESS RESECTION TO AVOID UNNECESSARY COLORECTAL SURGERY
Phillip S. Ge*, Gottumukkala S. Raju, Emmanuel Coronel, Deanndra N. Casanova, Brian K. Bednarski, Tsuyoshi Konishi, Craig A. Messick, Oliver Peacock, Miguel A. Rodriguez-Bigas, John M. Skibber, Abhineet Uppal, Y. Nancy You, George J. Chang, Matthew M. Tillman
The University of Texas MD Anderson Cancer Center, Houston, TX
Background: Piecemeal or incomplete resection of malignant polyps found on colonoscopy is a common reason for patients to be referred for colorectal surgical consultation due to risks of local recurrence as well as regional/distant metastasis. When the index lesion is resected in piecemeal or incomplete fashion, tumor (T)-staging cannot be properly assessed (pTx). Traditionally, surgical resection was offered as the standard of care to establish proper staging and ensure complete oncological resection. Alternatively, colonoscopic endoscopic full thickness resection (cEFTR) may provide an organ-sparing alternative to surgery, and help further define the depth of tumor invasion, thus establishing formal T-staging, with added possibility of complete oncological resection. Here we report our experience with staging cEFTR within a multidisciplinary colorectal practice at a major US-based academic cancer center.
Methods: We analyzed consecutive patients with piecemeal or incomplete resection of malignant colorectal polyps or neuroendocrine tumors (NET) who were referred to our group for staging cEFTR using a dedicated full thickness resection device (FTRD) since its introduction at our institution in August 2020. Demographics, procedural and technical characteristics, resection outcomes, adverse events, and final histopathologic diagnosis were recorded.
Results: 18 staging cEFTR cases were identified, which included 1 right colon, 2 left colon, and 15 rectal lesions. Mean patient age was 57.1 years, with 50.0% female. Nine of the 18 staging cEFTR cases were from piecemeal or incomplete resection of submucosally-invasive adenocarcinoma, and the other 9 were from piecemeal or incomplete resection of neuroendocrine tumors (NET). cEFTR was performed exclusively in the outpatient setting, and none required hospitalization. Overall, complete (R0) resection and curative resection were achieved respectively in 100% and 88.9% cases. Adverse events included 1 case each (2.5%) of tenesmus, perineal pain, and minor delayed bleeding which was endoscopically managed in the outpatient setting. Histopathology showed 1 case with residual adenoma, 1 case with residual NET, and 2 cases with submucosally-invasive adenocarcinoma (pT1) with high-risk histopathological features. The remaining 14 cases showed no residual tumor, thus establishing formal pT1 staging. There were no recurrences at mean 5.7 month follow-up (SD, 1.6 months). One patient with pT1 adenocarcinoma with perineural invasion underwent formal surgical resection, and was found to have no residual disease.
Conclusions: Staging cEFTR represents a safe and effective outpatient and organ-sparing alternative to surgical resection, establishing formal tumor staging while avoiding unnecessary colorectal surgery. Ongoing studies with long-term follow-up will seek to further validate these findings.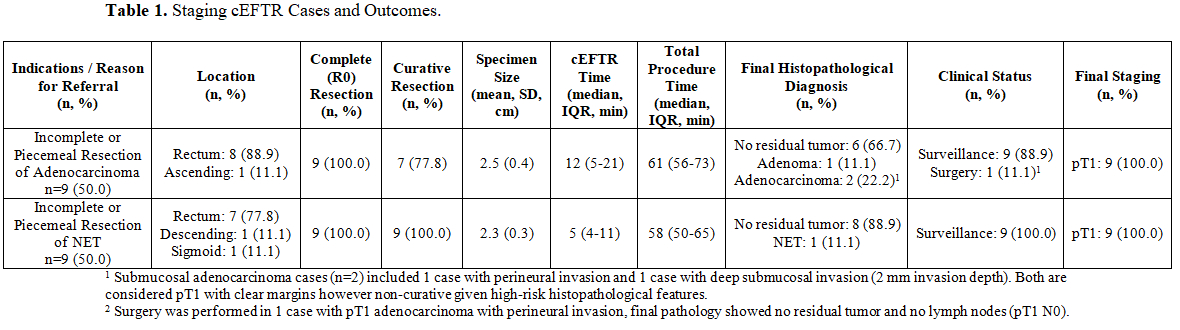
Table 1. Staging cEFTR Cases and Outcomes.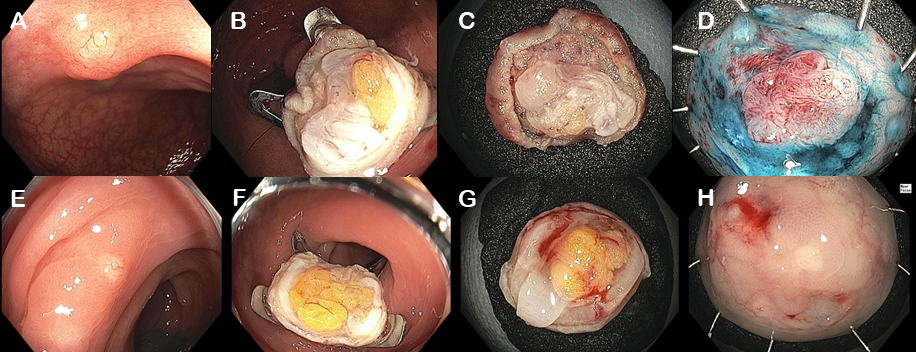
Figure 1: Staging cEFTR Cases. (A) cEFTR referral for incomplete resection of submucosally-invasive adenocarcinoma, demonstrating residual tumor on the resection scar. (B) cEFTR resection defect and (C, D) specimen. (E) cEFTR referral for incomplete resection of neuroendocrine tumor, demonstrating residual tumor on the resection scar. (F) cEFTR resection defect and (G, H) specimen.
Back to 2022 Posters
