UTILITY OF THE LÉMANN INDEX IN THE PREDICTION OF POSTOPERATIVE COMPLICATIONS IN HIGH RISK CROHN'S PATIENTS: A PROPENSITY SCORE MATCH ANALYSIS
Volkan Do?ru*, Michael J. Grieco, Umut Akova, Eren Esen, Arman Erkan, Andre da Luz Moreira, John Kirat, Feza H. Remzi
Inflammatory Bowel Disease Center, NYU Langone Health, New York, NY
Introduction
The Lémann Index (LI) is a validated tool which quantifies the extent of structural bowel damage in Crohn's disease. Although LI can predict the risk of early abdominal surgery in Crohn's disease, its utility in the prediction of postoperative complications has never been studied in depth before.
Methods
A one-to-one propensity score model was used to match high risk Crohn's patients with early major postoperative complications (Clavien-Dindo ?3 and/or the suffix "d" for disability) to control patients (Clavien-Dindo <3). Patients were included only if they were identified as being at high risk for sepsis or abdominal catastrophe requiring fecal diversion. A hypothetical scenario to illustrate the steps in calculating the Lémann Index in a Crohn's patient is presented in Table 1.
Results
A total of 176 patients met inclusion criteria. With 20 (11%) patients developing Grade ?3 complications and 34 (19%) developing lower-grade but some form of a residual disability at discharge, the major complication group was older (median 43 vs. 33 years; IQR 32-57 vs. 24-45; p<0.001), had a higher average of ASA level (median 2 vs 2; IQR 2-3 vs 2-2; p<0.001) and had a higher Lemann index (median 26 vs 14; IQR 17-40 vs 9-25; p<0.001); whereas their surgery was more commonly a recurrent resection (54% vs 30%, p=0.002), they had more enterocutaneous fistulas (20% vs 9%, p=0.036) and iliopsoas abscess complicating Crohn disease (17% vs 7%, p=0.036). Perioperative malnutrition was also more common in the complication group (26% vs. 13%, p=0.037) and their operation was more commonly a conventional open surgery (67% vs 39%, p=0.001). The complication group was then well matched to controls for the aforementioned significant differences to examine the effect of Lemann Index. After propensity score matching, Lemann Index maintained its influence on postoperative major complications (OR 1.032, 95% Cl: 1,004-1,060, p=0,025). The optimal cut-off level was 16, with 80% sensitivity and 50% specificity (AUC=0.638; 95% CI: 0.533–0.742).
Discussion
Although it is difficult to estimate the extent of resections before the surgery for Crohn's, Lémann Index calculated at the end of the surgery may serve as a reliable tool to predict the postoperative complications of high risk Crohn's patients within the postoperative period. Such a predictor might be useful as an aid in continuity of care. Further study is warranted into the ability of a postoperatively calculated LI to predict the risk of postoperative complications.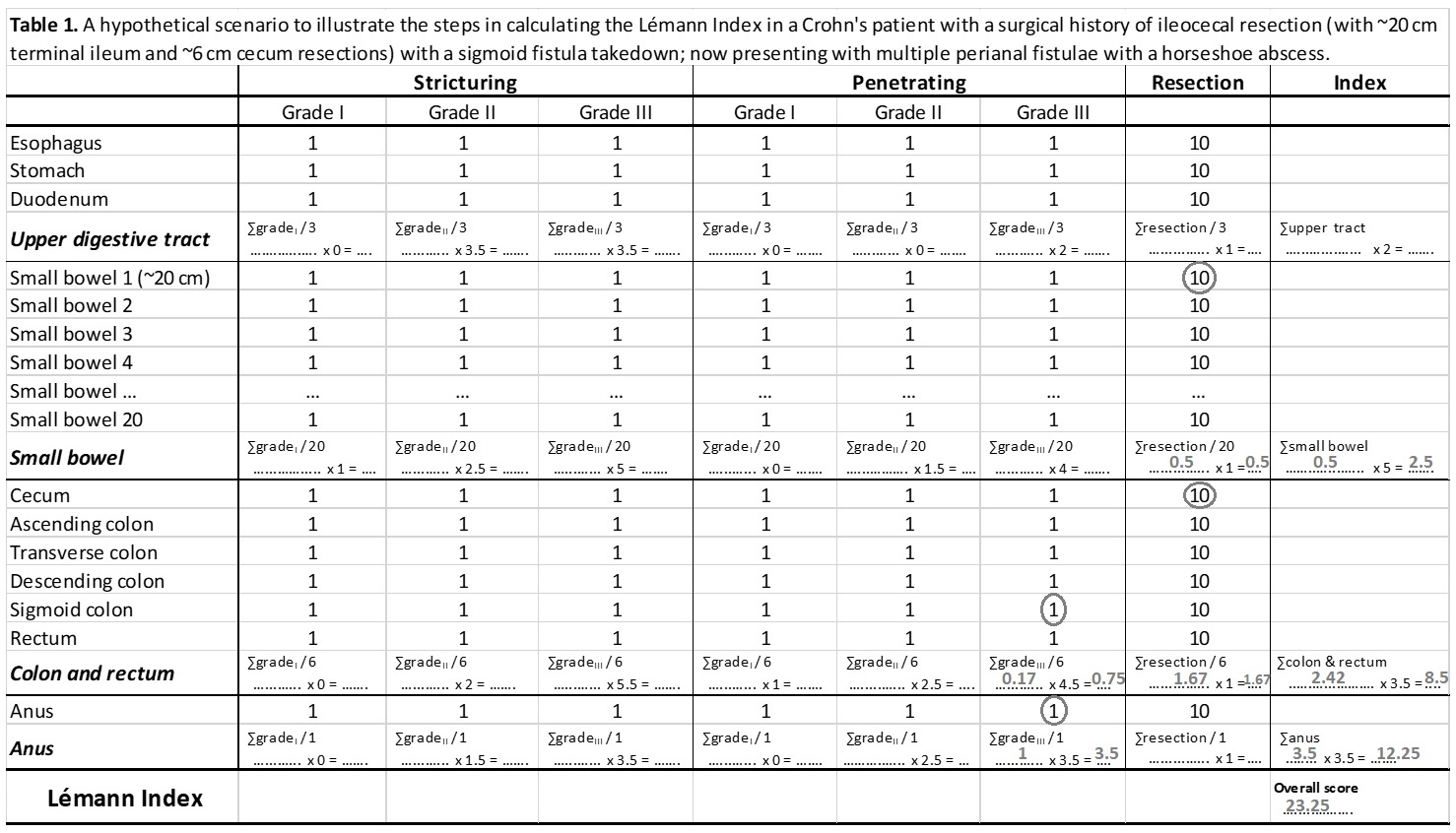
Back to 2022 Posters
