PREOPERATIVE ENDOSCOPIC RESECTION OF LARGE SYNCHRONOUS COLORECTAL NEOPLASIA LIMITS THE EXTENT OF SURGICAL RESECTION
Phillip S. Ge*, Gottumukkala S. Raju, Deanndra N. Casanova, Emmanuel Coronel, Brian K. Bednarski, Tsuyoshi Konishi, Craig A. Messick, Oliver Peacock, Miguel A. Rodriguez-Bigas, John M. Skibber, Abhineet Uppal, Y. Nancy You, George J. Chang, Matthew M. Tillman
The University of Texas MD Anderson Cancer Center, Houston, TX
Background: Synchronous neoplasia are often left unresected when patients are referred for surgical resection for colorectal cancer (CRC), typically due to uncertainty with regards to surgical planning. However, the resection of large synchronous polyps may directly influence the extent of surgical resection, affording patients the possibility of having a smaller resection with less impact to quality of life. Here we report our experience with endoscopic submucosal dissection (ESD) for preoperative endoscopic resection of synchronous colorectal neoplasia within a multidisciplinary colorectal practice at a major US-based academic cancer center.
Methods: We analyzed consecutive patients undergoing ESD for synchronous colorectal neoplasia over a 3-year period from 2018-2021 from a prospectively-collected endoscopic resection database. Demographics, procedural and technical characteristics, lesion characteristics, resection outcomes, and histopathologic diagnosis were recorded. Adverse events including perforation, bleeding, stricture, and recurrence were evaluated.
Results: A total of 18 lesions in 16 patients were identified, which included 15 right colon, 1 left colon, and 2 rectal lesions. Mean lesion size was 4.9 cm (SD, 1.7 cm). Mean resection time was 90.6 min (SD, 44.4 min), and mean resection speed of 12.0 cm2/hr (SD, 4.1 cm2/hr). En bloc resection, complete (R0) resection, and curative resection were achieved respectively in 88.9%, 88.9%, and 83.3% cases. Adverse events included 1 case of delayed bleeding which was successfully managed endoscopically. No patients required emergency surgery. In patients who have undergone subsequent follow-up, there were no recurrences at mean 13.2 month follow-up (SD, 4.7 months). A total of 12 patients (75.0%) ultimately underwent a much-smaller definitive surgical resection, and 2 patients (12.5%) were able to undergo a "watch-and-wait" surveillance altogether for complete clinical response of their primary CRC from chemoradiotherapy.
Conclusions: Preoperative endoscopic resection of synchronous large polyps in patients with CRC provides an opportunity to undergo a smaller definitive surgical resection, with ability to preserve more colon and thus with less impact to quality of life. Larger studies with long-term follow-up will seek to further validate these findings.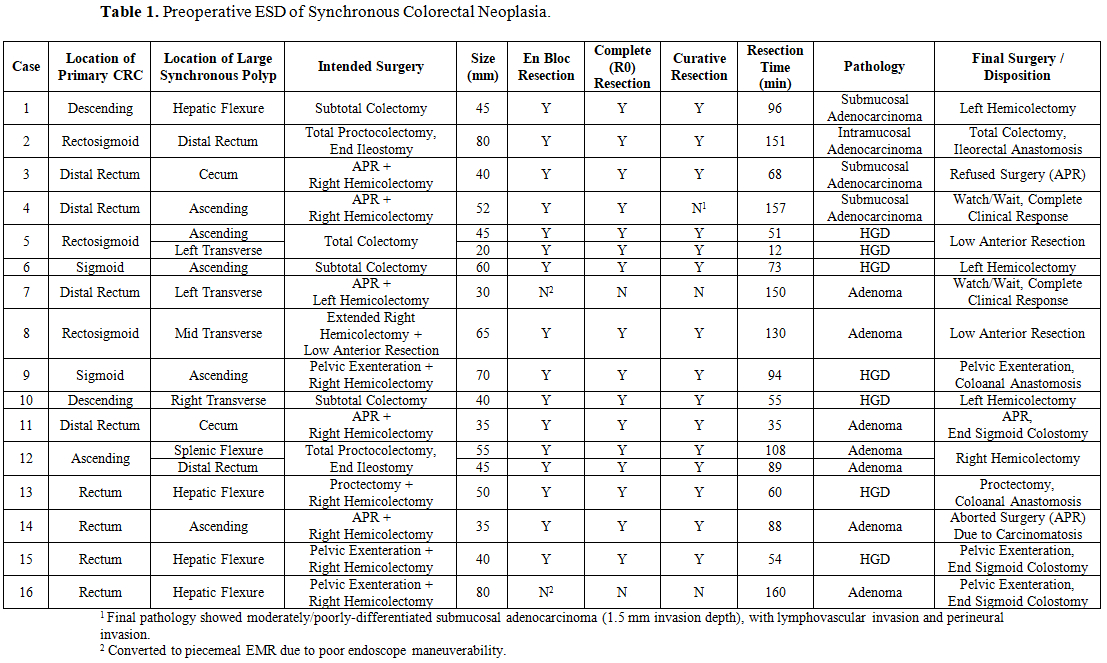
Table 1. Preoperative ESD of Synchronous Colorectal Neoplasia.
Figure 1: Preoperative ESD of Synchronous Colorectal Neoplasia. (A) A patient with rectal adenocarcinoma with a (B) synchronous large synchronous hepatic flexure polyp, who was originally planned for proctectomy vs abdominoperineal resection with additional right hemicolectomy. (C, D) ESD was performed. (E) ESD resection defect and (F) specimen. A curative resection was achieved and the patient ultimately underwent a proctectomy with coloanal anastomosis.
Back to 2022 Posters
