EFFECT OF GASTRIC CONDUIT MORPHOLOGY ON PERFUSION USING INDOCYANINE GREEN FLUORESCENCE ANGIOGRAPHY IN ESOPHAGECTOMY
Yoshitaka Ishikawa*, Andrew C. Chang, Jules Lin, Mark B. Orringer, William R. Lynch, Kiran H. Lagisetty, Elliot Wakeam, Rishindra M. Reddy
Thoracic surgery, University of Michigan Health System, Ann Arbor, MI
Purpose
There are many ways to shape the gastric conduit during an esophagectomy; however, it is not clear what is the ideal shape of the gastric conduit. Fluorescence angiography allows for the analysis of arterial inflow and venous outflow to measure the health of the conduit, which can impact leak after surgery. The aim of this study is to evaluate effects of gastric conduit morphology on its perfusion and an incidence of anastomotic leak after esophagectomy.
Methods
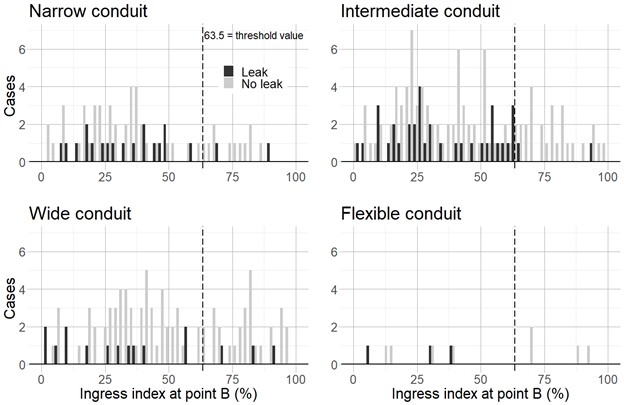
Patients from a single, high volume, esophagectomy center who underwent a transhiatal or 3-field esophagectomy between July 2015 and June 2021 were evaluated . Patients' demographic, surgical technique, histopathology, conduit measurement, conduit perfusion, and postoperative outcomes after esophagectomy were analyzed. Indocyanine green (ICG) fluorescence angiography was performed to evaluate gastric conduit perfusion. Ingress index (arterial inflow) and estimated ingress time and egress curve presence, which reflect venous outflow, were measured (Figure 1). Patients were classified into four groups according to a width of the conduit: narrow conduit (the middle of the conduit <4 cm), intermediate conduit (4?, <5 cm), wide conduit (5 cm?), and flexible conduit (the tip is wider than the middle of the conduit) . Perfusion pattern was also grouped into four groups according to ICG fluorescence angiography: good inflow (ingress index ?63.5%) and good outflow (ingress time ?37.5 sec), good inflow and poor outflow (>37.5 sec), poor inflow (<63.5%) and good outflow, poor inflow and poor outflow. Fisher exact test (with Bonferroni correction), Mann-Whitney U test, Kruskal-Wallis test, and Steel-Dwass test were used to make statistical comparisons between the groups.
Results
Three hundred and twenty-two patients who underwent an esophagectomy were reviewed, and anastomotic leak occurred in 77 patients (23.9%). The conduit was significantly narrower in the leak group (4.4 vs 4.7 cm, p=0.019). Ingress index was lower (35.6 vs 45.0%, p=0.006) and ingress time was longer (66.4 vs 55.9 sec, p=0.016) in the leak group with significant differences. Only 5.4% in the good inflow and outflow group developed anastomotic leak with significant differences compared with the other perfusion patterns. Wide conduits had a significantly high ingress index compared with narrow conduits (48.3 vs 37.2%, p=0.020, Figure 2).
Conclusions
Wide conduits seem to have good inflow and outflow and might reduce anastomotic leak. However, the relationships between conduit shape, conduit perfusion, and anastomotic leak are not straight forward. More cases will be needed to determine the ideal conduit shape.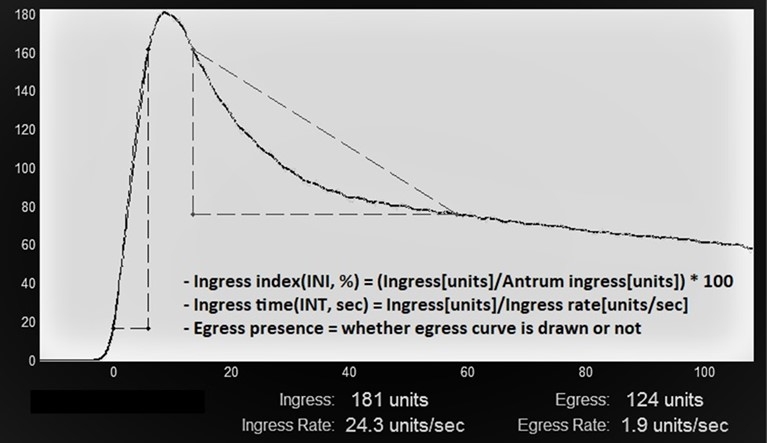
Back to 2022 Abstracts
