NECROTIZING PANCREATITIS-ASSOCIATED ANXIETY, DEPRESSION, AND STRESS: INCIDENCE, RISK FACTORS, AND TARGETS FOR INTERVENTION
Sean P. McGuire*, Thomas K. Maatman, Kathleen A. McGreevy, Anne Mary Montero, Michael G. House, Nicholas J. Zyromski
General Surgery, Indiana University System, Indianapolis, IN
Introduction: Anecdotally, depression is a commonly observed in necrotizing pancreatitis patients. However, objective evaluation of mental health in this disease has not been accomplished. We sought to prospectively quantify symptoms of anxiety, depression, and post-traumatic stress disorder (PTSD) in patients with necrotizing pancreatitis.
Methods: Adult patients with active necrotizing pancreatitis were prospectively screened for anxiety using the General Anxiety Disorder-7 (GAD7), depression using the Patient Health Questionnaire-9 (PHQ9), and PTSD using the PTSD Checklist for DSM-5 (PCL5).
Results: Fourteen patients were screened at an average of 109 days (IQR 58-142) after disease onset. Positive screening for anxiety and depression was extremely common: 71% met criteria for anxiety and 79% met criteria for depression (Figure 1). PTSD was less common (14%) at this screening timepoint. Prior mental health diagnoses, time from disease onset to screening, readmission profile, and mechanical intervention profile were not risk factors for the development of anxiety, depression, or PTSD symptoms. Patients diagnosed with anxiety and/or depression had more severe necrotizing pancreatitis: computed tomography severity index (CTSI) was higher in patients with anxiety (6.7 ± 2.1 vs 6.5 ± 1.0, p = 0.05) and depression (6.9 ± 2.0 vs 5.7 ± 0.6, p = 0.04). Infected necrosis, ICU admission, and organ failure were higher in patients with anxiety and depression though not reaching statistical significance (Figure 2). Patients are currently being enrolled in a mindfulness-based intervention.
Conclusions: Necrotizing pancreatitis carries a high risk of impaired mental health; those with severe disease are at highest risk. Directed treatment of anxiety and depression during the course of necrotizing pancreatitis has the potential to improve well-being and may impact disease course.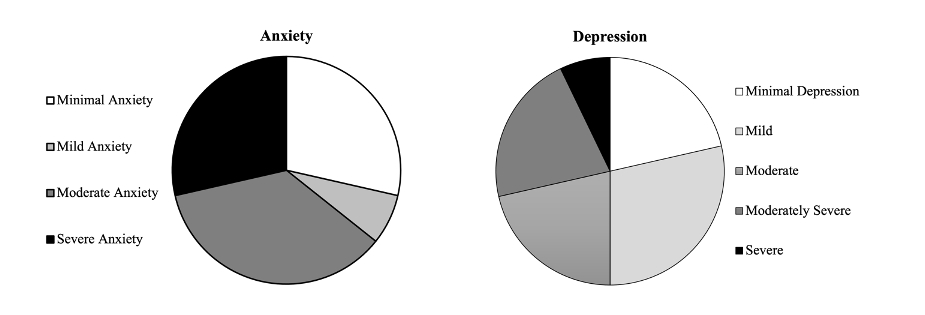
Figure 1: Severity of anxiety and depression symptoms in necrotizing pancreatitis patients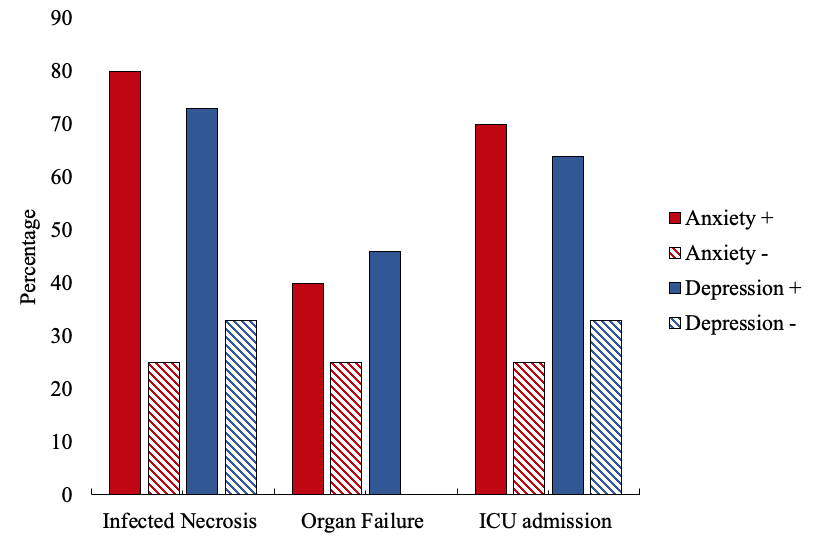
Figure 2: Variables associated with anxiety and depression in necrotizing pancreatits patients
Back to 2022 Abstracts
