PREOPERATIVE MALNUTRITION AND NUTRITIONAL SUPPORT AMONGST PATIENTS UNDERGOING MAJOR INFLAMMATORY BOWEL DISEASE SURGERY
Andrew T. Weber*1, Shaya Noorian2, Yejoo Jeon2, Renae A. Tessem3, Saloni Gupta3, Joseph Ebriani3, Michelle Nguyen4, Nancee Jaffe1, Jenny S. Sauk1, Mary Kwaan5, Berkeley N. Limketkai1
1University of California Los Angeles Division of Digestive Diseases, Los Angeles, CA; 2Ronald Reagan UCLA Medical Center, Los Angeles, CA; 3University of California Los Angeles David Geffen School of Medicine, Los Angeles, CA; 4Tufts University School of Medicine, Boston, MA; 5University of California Los Angeles Section of Colon and Rectal Surgery, Los Angeles, CA
Background
Surgery is frequently required amongst patients with inflammatory bowel disease (IBD) due to refractory disease and/or complications. Patients with IBD are at increased risk for protein-calorie malnutrition (PCM), a known risk factor for adverse postoperative outcomes. This study sought to evaluate the real-world prevalence of preoperative PCM in patients undergoing major IBD-related surgery, the impact of PCM on postoperative outcomes, and the frequency of preoperative nutritional support utilization.
Methods
We performed a retrospective study of adult patients who underwent major IBD-related surgery at a single tertiary referral center between 2010 and 2021. The medical record was manually reviewed to identify evidence of preoperative PCM and receipt of nutritional support prior to surgery. Multivariable logistic regression was utilized to analyze the effects of PCM on postoperative outcomes (wound infection, intra-abdominal infection, systemic infection, 30-day reoperation, 30-day readmission), adjusting for demographics, medication use, medication response, elective surgery, and open or laparoscopic surgery.
Results
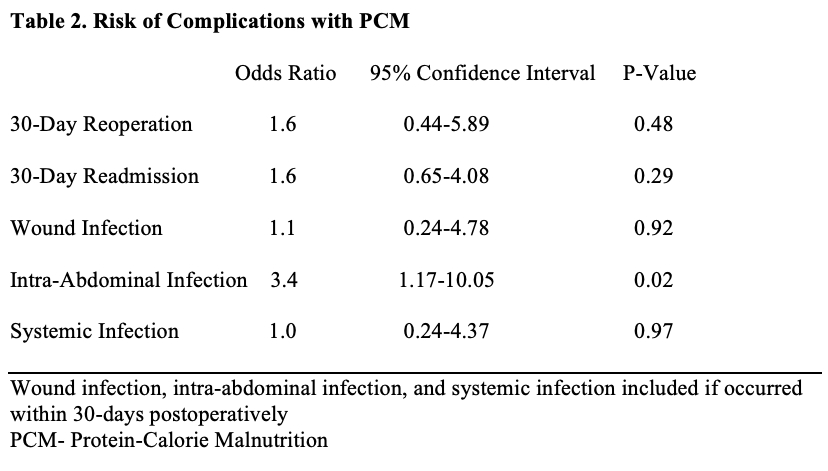
267 patients underwent major IBD-related surgery between 2010 and 2021. Of these patients, 112 (42%) had evidence of preoperative PCM while 155 (58%) had no preoperative PCM. Preoperative PCM was more common in younger patients (37.6 years vs. 43.5 years, p < 0.01) and those experiencing medication failure (55.4% vs. 33.5%, p=0.01), on steroids (60.4% vs. 43.4%, p=0.01), and undergoing non-elective surgery (35.8% vs. 19.7%, p<0.01). Demographic and disease-specific variables were otherwise well balanced between patients with and without PCM (Table 1). On multivariable logistic regression with adjustment for potential confounders, PCM was associated with increased likelihood of postoperative intra-abdominal infection (OR 3.43, p=0.02) but not wound infection (OR 1.08, p=0.92), systemic infection (OR 1.02, p=0.97), 30-day reoperation (OR 1.6, p=0.48), or 30-day readmission (OR 1.63, p=0.29) (Table 2). Amongst the 112 patients with PCM, 34 (30.4%) received preoperative enteral nutrition, while 26 (23.2%) received preoperative parenteral nutrition. 52 patients (46.4%) with PCM received no preoperative nutrition support. Preoperative assessment by Nutrition occurred in 53 patients (47.3%) with PCM. 49 patients (34.8%) with PCM received neither preoperative nutrition support nor Nutrition assessment.
Conclusions
In our retrospective study from a tertiary referral center, PCM was common prior to major IBD-related surgery and associated with increased risk of postoperative complications but inconsistently intervened upon. Providers should be vigilant for underlying PCM in patients with IBD pending surgery and should remain proactive in ensuring PCM is appropriately addressed once identified to improve overall perioperative outcomes.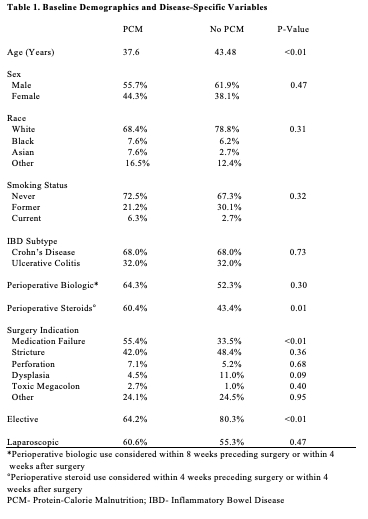
Back to 2022 Abstracts
