LOW MOLECULAR WEIGHT HEPARIN USE AND THROMBOTIC COMPLICATIONS IN UPPER GASTROINTESTINAL RESECTION FOR MALIGNANCY IN A MULTI-ETHNIC ASIAN POPULATION
Lydia L. Tan*1, Xuan Gleaves1, Prabhu Nesargikar1, Shen Liang2, Asim Shabbir1, Guo Wei Kim1, Jimmy B. So1
1General Surgery, National University Health System, Singapore, Singapore; 2National University of Singapore, Singapore, Singapore
Objective: Epidemiological studies have shown a substantially lower venous thromboembolic event risk in Asians compared to Caucasians. There is no guideline in Asia regarding the thromboprophylaxis in patients with malignant disease undergoing major surgery. Hence, postoperative use of low molecular weight heparin (LMWH) in upper gastrointestinal (UGI) surgery in Singapore is based on surgeons' discretion.
Methods: A retrospective study of all upper gastrointestinal resections for malignancy performed in a tertiary institution in Singapore was included for this study. Basic demographics, clinicopathological data and treatment outcome data were collected and analysed.
Results: A total of 400 UGI resections for cancers performed between year 2008 and 2018 were included in the study. 212 patients received postoperative LMWH, while 188 patients did not have postoperative LMWH. Basic demographics such as age, gender, BMI, smoking status were comparable. In the study cohort, 63.5% were American Society of Anaesthesiology score 2. Most cancers were stage 3 (42.5% in no LMWH group and 34.3% in LMWH group). Patients who had open surgery were more likely to receive postoperative LMWH, with 67.2% undergoing open surgery in the no LMWH group vs 81.1% undergoing open surgery in the LMWH group (p value = 0.001). Postoperative mortality (3.2% in patients with no LMWH use vs 2.8% in patients with LMWH use) and rate of venous thromboembolic events (1.6% in patients with no LMWH use vs 1.4% in patients with LMWH use) were similar in both groups of patients. However, use of postoperative LMWH was associated with increase need for blood transfusion (21.1% in patients with no LMWH use vs 39.6% in patients with LMWH use, with p value < 0.001) and reoperation secondary to bleeding (0.5% in patients with no LMWH use vs 2.8% in patients with LMWH use, with p value = 0.079). Multivariate analysis showed that patients with LMWH had significantly higher risk of blood transfusion needed after surgery.
Conclusion: Incidence of symptomatic deep vein thrombosis or pulmonary embolism was similar in patients who received postoperative LMWH and patients who did not. However, LMWH use was associated with increased risk of postoperative bleeding. Hence, routine LMWH may not be required for patients undergoing UGI resection for malignant disease in our population.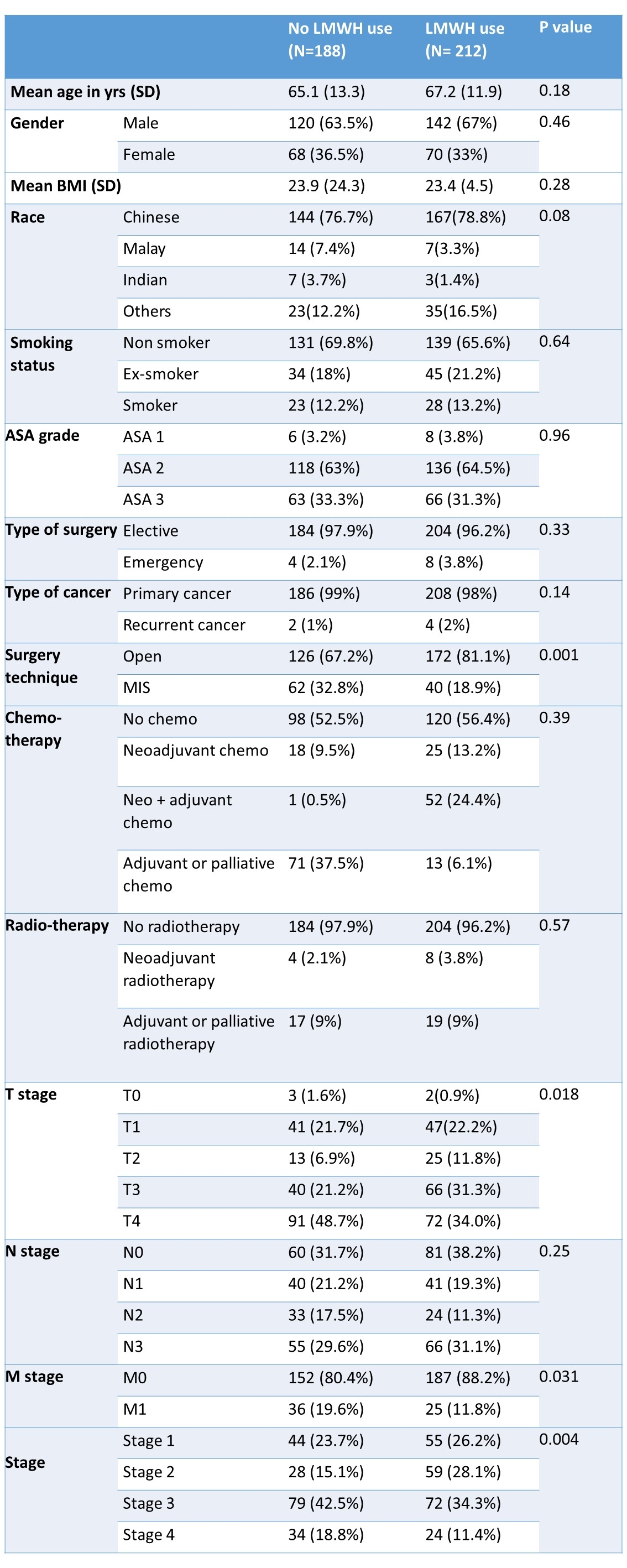
Table 1: Demographics of patients with no postoperative LMWH use vs patients with postoperative LMWH.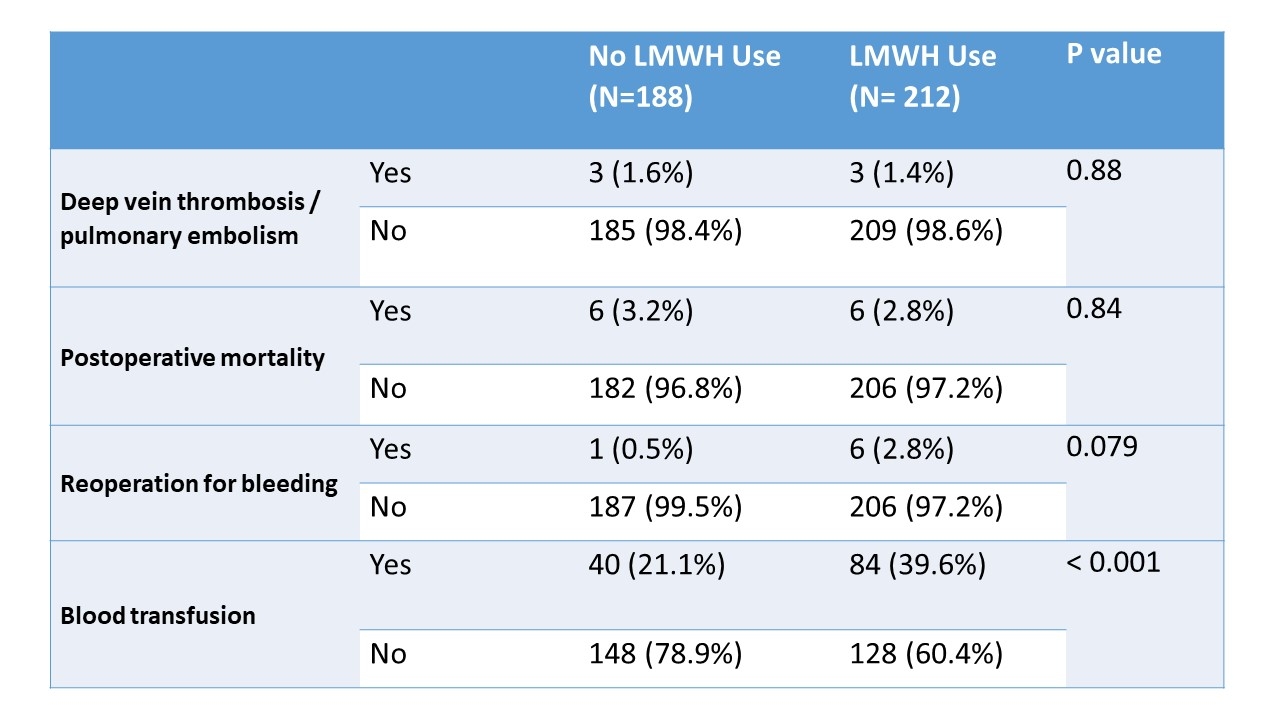
Table 2: Outcomes of patients with no postoperative LMWH use vs patients with postoperative LMWH use.
Back to 2022 Abstracts
