ENDOSCOPIC VACUUM THERAPY FOR PATIENTS WITH ANASTOMOTIC LEAKAGE AFTER ESOPHAGO-GASTRIC SURGERY
Lisanne M. Pattynama*, Roos E. Pouw, Mark I. Van Berge Henegouwen, Freek Daams, Suzanne S. Gisbertz, Jacques Bergman, Wietse J. Eshuis
Amsterdam Universitair Medische Centra, Amsterdam, Noord-Holland, Netherlands
Introduction
Anastomotic leakage (AL) after upper gastro-intestinal (UGI) surgery is associated with severe morbidity and mortality. Recently endoscopic vacuum therapy (EVT), using an endoscopically placed sponge, was introduced as treatment of AL. The aim of this study was to describe the outcomes of the initial experiences with EVT in a tertiary referral center, in the treatment of AL after esophago-gastric surgery.
Patients and methods
For this retrospective cohort study, all patients treated with EVT for AL in the UGI tract at a tertiary referral center, between January 2018 and October 2021, were included. In this period patients with AL, based on CT-scan or endoscopic findings, were primarily treated with EVT. Cases were identified from the endoscopy reporting system, with a search including all available terms for EVT. Data on patient characteristics, EVT and outcomes were analyzed. The primary endpoints were success rate of EVT alone, defined as closure of the defect assessed by endoscopy or CT-scan, and severe complications.
Results
A total of 38 patients were included, of whom 31 (82%) were men. The mean age was 66 years (SD 9.3) (Table 1). Twelve patients had undergone a total gastrectomy with an esophago-jejunal anastomosis and 26 patients an esophageal resection with an esophago-gastric anastomosis (21 intrathoracic and 5 with a cervical anastomosis). Successful treatment with EVT was achieved in 28 patients (74%). In 10 patients EVT failed: one patient deceased during treatment (due to radiation pneumonitis) and 9 patients underwent additional surgery: one due to a tracheo-esophageal fistula, one because of iatrogenic expansion of the defect during overtube placement and 7 because defect closure was not achieved.
Median hospital stay was 42 days (range 14-160, IQR 2). Median duration of EVT was 27 days (range 6-88, IQR 34), with a median of 6 EVT-related endoscopies (range 2-19, IQR 8) and 5 days between sponge exchanges (range 1-9, IQR 3). Additional percutaneous drainage was performed in 22 patients (58%). EVT associated complications occurred in two patients (5%): in one patient the overtube caused iatrogenic expansion of the defect and one developed a tracheo-esophageal fistula.
Conclusion
EVT is a paradigm shifting treatment potentially preventing surgical re-intervention in patients with AL after UGI surgery, with a success rate of 74%. More experience with the technique and indications for use will likely improve success rates in the future.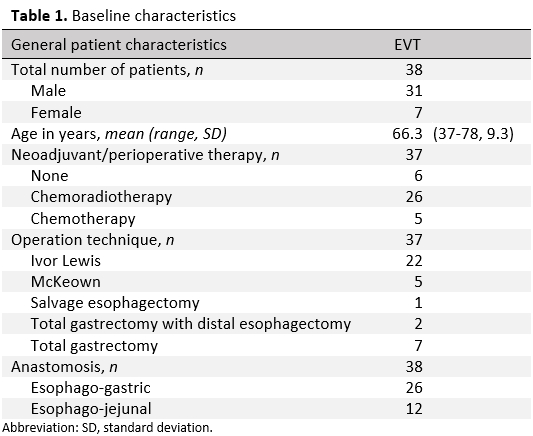
Table 1. Baseline characteristics
Back to 2022 Abstracts
