INEFFECTIVE ESOPHAGEAL MOTILITY: THE IMPACT OF CHANGE OF CRITERIA IN CHICAGO CLASSIFICATION VERSION 4.0 (CCV4.0) ON PREDICTING SURGICAL OUTCOME
Margaret Riccardi*1, Steven Tamesis1, Ping Zheng1, Sven Eriksson1, Ashten N. Omstead1, Blair Jobe1,2, Shahin Ayazi1,2
1Esophageal Institute, Department of Surgery, Allegheny Health Network, Pittsburgh, PA; 2Drexel University, Philadelphia, PA
Introduction: The Chicago Classification version 4.0 (CCv4.0) for interpretation of high resolution manometry (HRM) was recently introduced, and one of the major changes was the definition of ineffective esophageal motility (IEM). How this effects surgical outcomes is yet untested. We designed the current study to evaluate the impact of these new criteria on predicting dysphagia after magnetic sphincter augmentation (MSA).
Methods: The records of patients who underwent MSA from 2013 to 2020 in our center were reviewed. Those who completed their pre-operative HRM in our institution and had at least one year of follow-up were selected. HRM files of these patients were reanalyzed by two investigators and patients were classified as IEM based on Chicago 3 (CCv4.0) or Chicago 4 (CCv4.0) guidelines (Figure 1). Immediate dysphagia was defined as any difficulty swallowing within the first 6 weeks after surgery. Persistent dysphagia was defined as a score of >3 for the dysphagia-specific item within the GERD-HRQL at one year following surgery. Statistical analysis was performed to assess for accuracy, positive predictive value (PPV), negative predictive value (NPV), and C statistic (area under the curve) to compare dysphagia outcomes predicted by CCv3.0 and CCv4.0.
Results: A total of 336 patients (63% female) met the inclusion criteria. There was an overall improvement in GERD-HRQL score [34.0 (19.4) vs. 9.0 (11.6), p=0.002) and 91% of patients were off PPI following surgery. Forty two patients (12.5%) were found to have persistent dysphagia at one year follow-up.
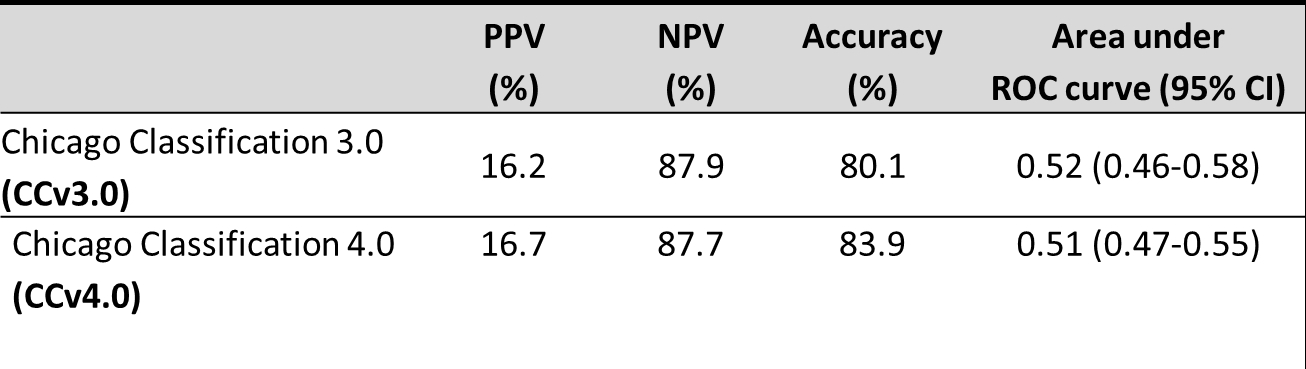
Based on CCv3.0 and CCv4.0, a total of 37 (11%) and 18 (5.4%) patients were classified with IEM respectively. Neither classification was an accurate predictor of immediate dysphagia (46.1% and 44.1%). For persistent dysphagia, there was no significant difference in PPV, NPV or accuracy between CCv3.0 and CCv4.0 (Figure 2). When evaluating the individual components of CCv4.0, ? 50% failed swallows was the most predictive, with accuracy of 87.2%, PPV of 40%, and NPV of 87.92%. Abnormal bolus clearance defined as bolus clearance < 80% was more predictive of dysphagia than the other components of CCv4.0. With the combination of CCv4.0 and abnormal bolus clearance of < 80% accuracy was 86.3%, PPV 30%, and NPV of 88.04%.
Conclusion: Neither classification was predictive of immediate dysphagia which is consistent with prior findings as this is an expected outcome of the surgery itself and more subjective than persistent dysphagia. While CCv4.0 is more stringent with the increase to 70% ineffective swallows or 50% failed peristalsis from the prior 50% ineffective swallows, it does not have a statistically significant impact on predicting postoperative dysphagia. One consideration for a future definition of IEM would be the addition of a bolus clearance threshold to the definition of IEM.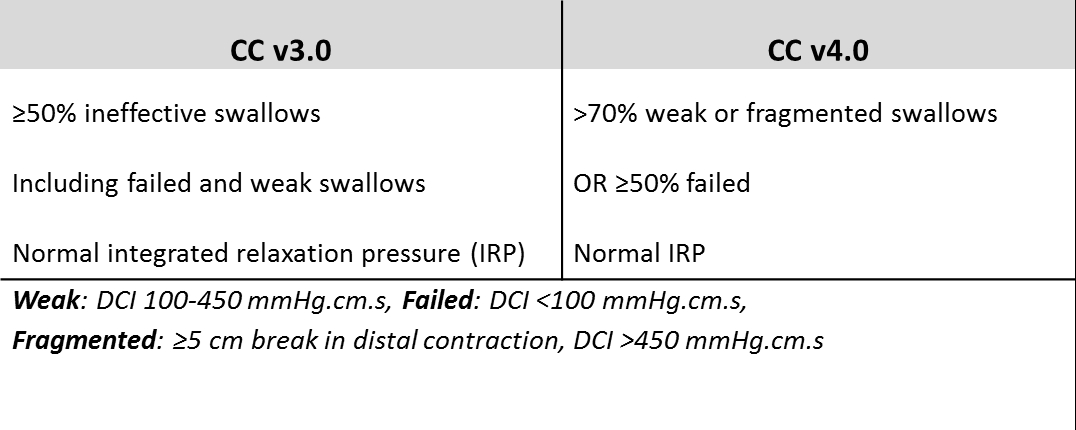
Back to 2022 Abstracts
