POST-OPERATIVE COMPLICATIONS IN IBD PATIENTS RECEIVING COMBINATION BIOLOGIC AND THIOPURINE THERAPY VERSUS BIOLOGIC MONOTHERAPY
Shaya Noorian*1, Andrew T. Weber1, Yejoo Jeon1, Renae A. Tessem2, Saloni Gupta2, Joseph Ebriani2, Michelle Nguyen3, Mary Kwaan1, Jenny S. Sauk1, Berkeley N. Limketkai1
1UCLA Medical Center, Los Angeles, CA; 2University of California Los Angeles David Geffen School of Medicine, Los Angeles, CA; 3Tufts University School of Medicine, Boston, MA
Background
Recent prospective data suggest that the use of anti-tumor necrosis factor (anti-TNF) therapy in patients with inflammatory bowel diseases (IBD) prior to abdominal surgery does not lead to increased risk of wound infections or overall infections. However, it is still unclear whether the additive immunosuppressive effects of combination biologic and thiopurine therapy, which are frequently used in the treatment of IBD, confer a higher risk of post-operative complications.
Methods
We performed a retrospective medical record review to identify IBD patients undergoing IBD-related surgery at a tertiary care referral center between 2010 and 2021. Cohorts were divided into those who received biologic monotherapy (within 8 weeks before or 4 weeks after IBD surgery) and those who received biologic (within 8 weeks before or 4 weeks after IBD surgery) plus thiopurine (within 4 weeks of IBD surgery) therapy. Outcomes of interest were post-operative (within 30 days of IBD surgery) wound infection, intra-abdominal infection, systemic infection, other infection, wound dehiscence, and overall complications (composite of the aforementioned post-operative complications). Univariable and multivariable logistic regression analyses evaluated associations between use of combination vs. monotherapy and post-operative outcomes. Multivariable models additionally evaluated factors such as patient background characteristics (age, sex, race, body-mass index, tobacco use), IBD type, elective status of surgery, and surgical approach (open versus laparoscopic).
Results
We identified 88 patients who received biologic monotherapy and 60 patients who received combination biologic plus thiopurine therapy. Groups were similar in demographic factors, IBD type, biologic class received, surgery indication, elective status of surgery, and surgery method (Table 1). Observed rates of infectious complications, wound dehiscence, and overall complications were generally low (Table 2). In the multivariable regression model, combination therapy was not associated with a higher risk of overall complications when compared to biologic monotherapy. In this model, body mass index was associated with overall complications (OR 1.15; 95% CI 1.01-1.30; P=0.04). However, all other measured factors, including race, tobacco use, age, sex, IBD type, steroid use, surgery type, and elective status of surgery were not associated with differences in overall complications.
Conclusions
In this study, combination biologic and thiopurine therapy, as compared to biologic monotherapy, is not associated with an increased risk of post-operative infections, wound dehiscence, or overall complications in IBD patients undergoing inpatient IBD-related surgery.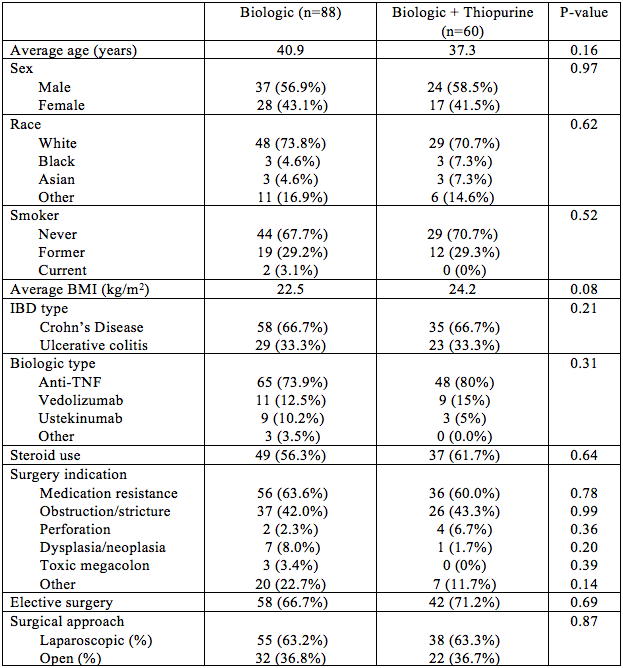
Table 1. Background Characteristics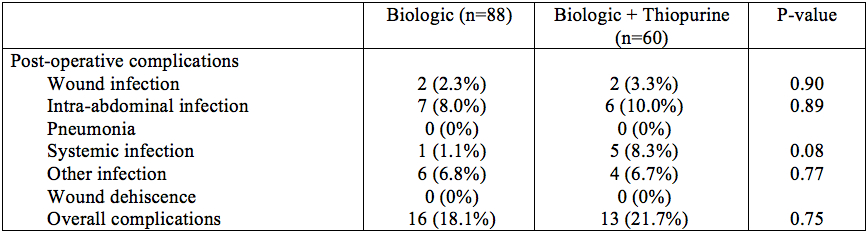
Table 2. Outcomes
Back to 2022 Abstracts
