RECURRENCE FOLLOWING COLORECTAL CANCER RESECTION IS ASSOCIATED WITH MICROBIAL RESISTANCE TO ANTIBIOTIC BOWEL PREPARATION
Ryan B. Morgan*, Julia Chael, Nicholas P. Dylla, Meejeon Roh, Eric Pamer, Olga Zaborina, Benjamin D. Shogan
The University of Chicago Medicine, Chicago, IL
Introduction: We have previously demonstrated that preoperative bacterial decontamination with a combined mechanical bowel preparation and oral antibiotics is associated with decreased rates of postoperative colorectal cancer (CRC) recurrence. The mechanism by which a combined bowel preparation protects against recurrence is unknown. In this study, we sought to test the hypothesis that patients who develop a CRC recurrence are resistant to the compositional changes induced by a preoperative combined bowel preparation.
Methods: Patients undergoing an operation with curative intent for CRC at a single institution were eligible for inclusion. All patients underwent a standardized bowel preparation one day before surgery with the laxative polyethylene glycol and the oral antibiotics neomycin and metronidazole. Stool samples were collected preoperatively (prior to receiving bowel preparation) and intraoperatively (after receiving bowel preparation). Samples were flash frozen at -80C. Microbial DNA was extracted using the QIAamp PowerFecal Pro DNA kit (Qiagen). Prior to extraction, samples were subjected to mechanical disruption with a bead beating method. Universal primers (563F and 926R) were used to PCR-amplify the hypervariable V4-V5 region of the 16S rRNA gene. Principle coordinate analyses (PCoA) were performed using Bray-Curtis dissimilarity distances to determine differences in microbial composition, ?-diversity, between preoperative and intraoperative samples and between patients who developed a CRC recurrence and those that did not. The absolute change in concentration of bacteria in each sample was determined by QT-PCR.
Results: 19 patients were included in the study. After a mean follow up of 26.4 months (range 22-32 months), 4 patients (21%) have developed a postoperative recurrence. When comparing intraoperative samples to preoperative samples, antibiotic decontamination significantly decreased bacterial composition (?-diversity, Bray-Curtis >0.4) in patients that did not develop a CRC recurrence (p<0.01); there was no change in the ?-diversity in patients who did develop a recurrence, indicating that preoperative decontamination had little impact on the gut microbiota of patients who developed a recurrence [FIG 1]. In addition to compositional changes, QT-PCR demonstrated that bacterial decontamination resulted in a 1000-fold decrease in bacterial concentration in patients that did not develop a recurrence; strikingly, patients who developed a recurrence showed almost no change in the amount of bacteria present before and after decontamination.
Conclusion: Postoperative CRC recurrence is associated with resistance of the intestinal microbiome to preoperative bacterial decontamination. Further investigation is necessary to determine the mechanism by which microbes that persist following bowel prep can promote postoperative CRC recurrence.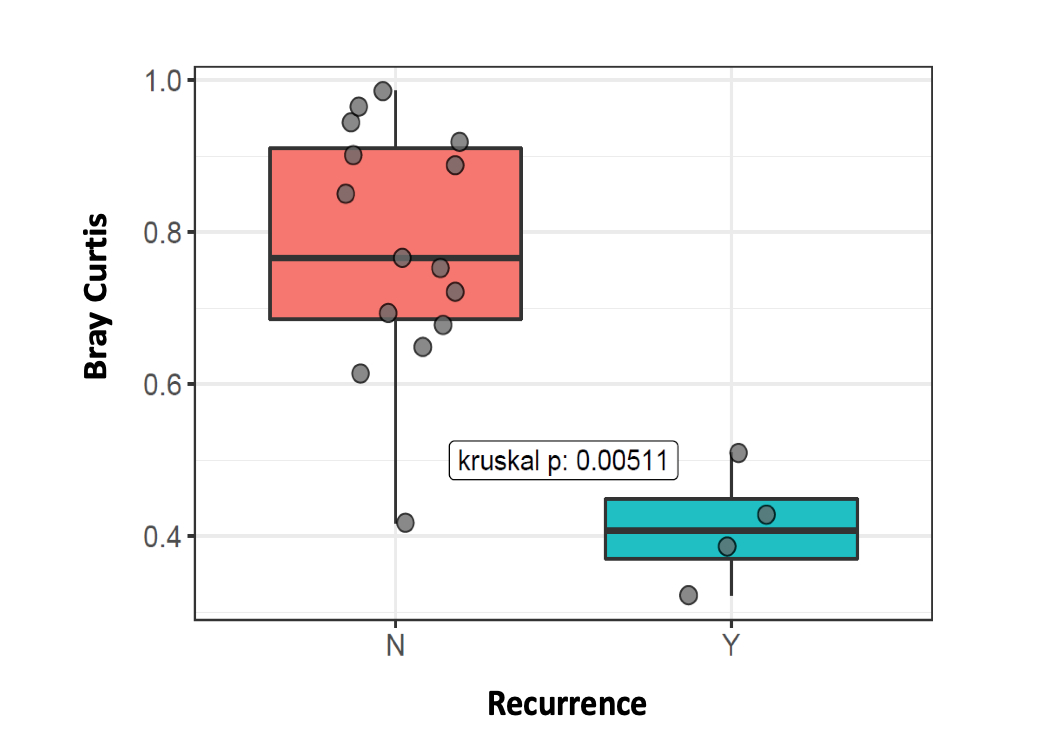
Figure 1: ?-diversity (Bray-Curtis dissimilarity) was significantly increased in matched preoperative and intraoperative stool samples from patients who did not develop postoperative CRC recurrence, whereas those who did have a recurrence demonstrated relatively minimal ?-diversity (p<0.01; Kruskal-Wallis test).
Back to 2022 Abstracts
