TRANSRECTAL ULTRASOUND (TRUS): AN ACCURATE AND INVALUABLE TOOL FOR IDENTIFYING SUITABLE CANDIDATES FOR TRANSANAL EXCISION/TRANSANAL ENDOSCOPIC MICROSURGERY (TAE/TEM) IN EARLY-STAGED RECTAL TUMORS
Charlotte H. Campbell*1, Jason Conway1, Doug Case2, Laura E. Lavette3, Darius A. Jahann1, Gregory S. Waters4, Jean Ashburn4, Alton Sutter4, Girish Mishra1
1Dept Gastroenterology and Hepatology Wake Forest Baptist Medical Center, Winston Salem, NC; 2Dept Public Health Sciences Wake Forest Baptist Health, Winston Salem, NC; 3Wake Forest University School of Medicine, Winston-Salem, NC; 4Dept Surgery Wake Forest Baptist Medical Center, Winston Salem, NC
Background & Aims: Assessing the depth of invasion for large, low-lying rectal lesions is absolutely critical in helping guide a complete, yet least invasive resection obviating the need for APR for lesions in proximity of the sphincter muscles. Preoperative staging of rectal tumors with MRI has supplanted TRUS worldwide, yet this can be less accurate in lesions near the anal sphincters. We hypothesize that TRUS can accurately identify low-lying rectal tumors that can achieve R0 resection via TAE/TEM.
Methods: All patients undergoing TRUS from January 2011 through December 2020 for evaluation of a rectal lesion were identified. Patients with adenomatous polyps, carcinoma in situ, or adenocarcinoma on pathology were included; other patients with benign pathology, surveillance TRUS, or non-carcinomatous malignancy were excluded. The rectal lesions were staged using the TNM staging system from the American Joint Committee on Cancer (2018). Preoperative staging with TRUS, lesion characteristics including size, demographics, operative interventions, and postoperative pathologic staging were assessed. The ability of TRUS to distinguish T0/Tis (deemed appropriate for TAE/TEM) vs ?T1 was noted. Pre- and postoperative staging was considered in agreement if both categorized a lesion as T0/Tis or if both were ?T1. Procedures were categorized as TAE/TEM, LAR, or APR. Test characteristics (sensitivity, specificity, positive and negative predictive value) were calculated to describe the preoperative staging with TRUS.
Results: 624 patients underwent an initial, staging TRUS. Patients with missing data or non-adenomatous/malignant pathology were excluded. 371 patients were identified (median age=64; range=19-96) with the average lesion size 3.76 cm [0.3cm-15.0cm]. Operative data was available on 264 patients with post-operative pathology on 175 patients. Test characteristics for TRUS include the following: Agreement=0.90; Sensitivity=0.96; Specificity=0.84; PPV=0.88; NPV=0.94, with no differences based on gender, age (<65 vs 65+) or lesion size (<3.0cm vs 3+cm). Test characteristics for patients undergoing TAE/TEM include: Agreement=0.96; Sensitivity=0.90; Specificity=0.98; PPV=0.97; NPV=0.95. Agreement (p=0.04), specificity (p<0.001), and PPV (p=0.038) were better for those patients undergoing TAE/TEM vs other modalities. No patient that underwent an APR had a T0/Tis on TRUS.
Conclusions: In this large, single-center study, we report phenomenal success using TRUS in determining which patients should undergo a TAE/TEM procedure (PPV and NPV=0.97 and 0.95 respectively). Over 98% of patients staged T0/Tis were <T2. Furthermore, no patients undergoing an APR had T0/Tis disease including lesions close to the anal sphincters, which can be challenging to visualize on MRI. TRUS is a critical component in the armamentarium for managing rectal tumors.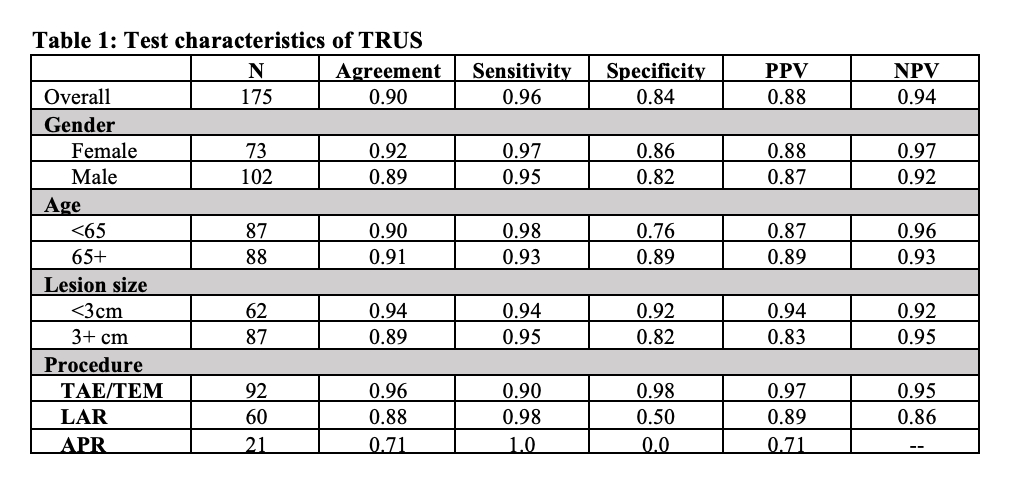
Back to 2022 Abstracts
