EVALUATION IN A MULTIDISCIPLINARY CLINIC INCREASES TREATMENT AND ELIMINATES SOCIOECONOMIC SURVIVAL DISPARITIES FOR PANCREATIC CANCER: A REGIONAL HOSPITAL SYSTEM ANALYSIS
Caroline Rieser*1, Richard S. Hoehn2, Mazen S. Zenati1, Kenneth Lee1, Alessandro Paniccia1, Amer H. Zureikat1
1Surgery, UPMC, Pittsburgh, PA; 2University Hospitals, Cleveland, OH
Background: National studies suggest pancreatic cancer patients receive surgery and indicated therapies at surprisingly low rates. Social determinants of health such as socioeconomic status (SES) have been shown to impact treatment and survival. We have previously shown that management by a pancreatic cancer multidisciplinary clinic (MDC) improves outcomes and eliminates socioeconomic disparities in survival for patients undergoing surgery. The aim of this analysis was to examine patient factors that predict referral to MDC and subsequent outcomes for all pancreatic cancer patients treated within a large regional health network.
Methods: We conducted a retrospective cohort study examining all patients diagnosed with pancreatic cancer from 2010-2018 at any of 15 hospitals in our network, including a high-volume pancreatic cancer center. Our primary exposure of interest was low SES as assessed by the national area deprivation index. Baseline patient characteristics, oncologic features, treatment strategies, and survival were also evaluated. Predictors of MDC referral were assessed by logistic regression.
Results: During the study period, 4,539 patients were identified with pancreatic cancer. Among these, 1,516 (33.4%) were evaluated in the MDC. Patients seen outside of the MDC were older (70 vs 69 years), less married (34% vs 45%), and had lower rates of private insurance (34% vs 43%; all p<0.001). On adjusted analysis, older age (OR 0.87 per decade), low SES (OR 0.78), travel distance (OR 0.54), and metastatic disease on diagnosis (OR 0.39) were all significant negative predictors of MDC assessment (all p<0.05). Marriage (OR 1.42) and private insurance (OR 1.23) were associated with MDC assessment (both p<0.001). On adjusted analyses, MDC was associated with higher odds of chemotherapy (OR 2.8), surgery (OR 1.75), and radiation treatment (1.89; all p<0.001). Additionally, there were higher odds of clinical trial participation (OR 3.92) and palliative care referral (OR 1.22; both p<0.001). Median survival was longer in the MDC compared to the non-MDC cohort (13.2 vs 5.9 mos, p<0.001). This persisted when examined by presence of metastatic disease at diagnosis (Figure 1). Examining by SES, outside of the MDC, high SES patients had improved survival (6.2 vs 4.1 mos, p<0.001). However, among patients treated within the MDC, there was no survival difference between high and low SES patients (13.6 vs 13.2 mos, p=0.97) (Figure 2).
Conclusions: This analysis is the first to evaluate barriers to MDC referral for patients with pancreatic cancer. We find that an interplay of patient and oncologic factors were associated with MDC assessment. MDC was also associated with higher rates of treatment and improved survival. Addressing barriers to MDC referral could improve care for patients with pancreatic cancer of all stages and help ensure more equitable outcomes.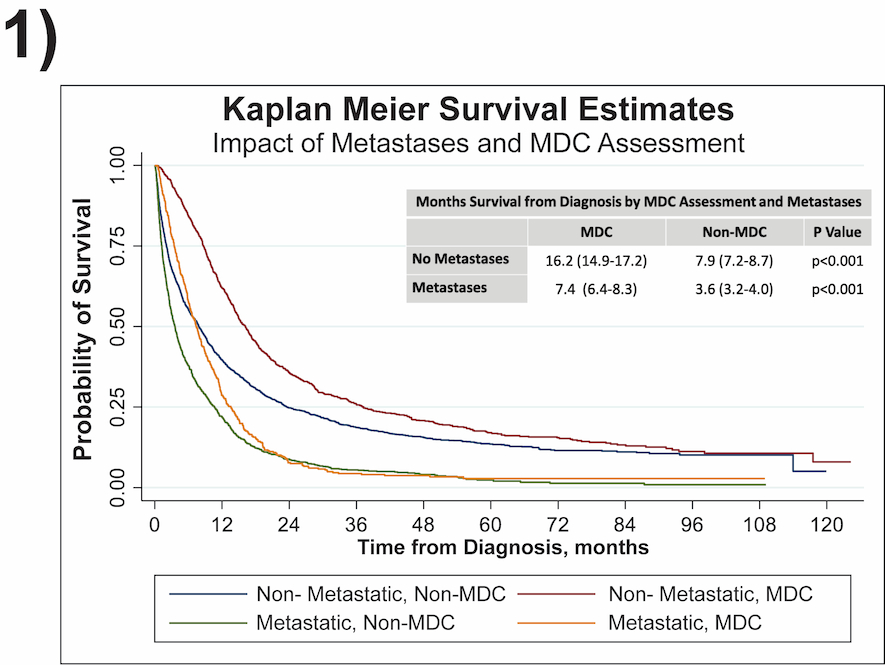
Survival from diagnosis (months) by multidisciplinary clinic (MDC) evaluation and presence or absence of metastases on diagnosis.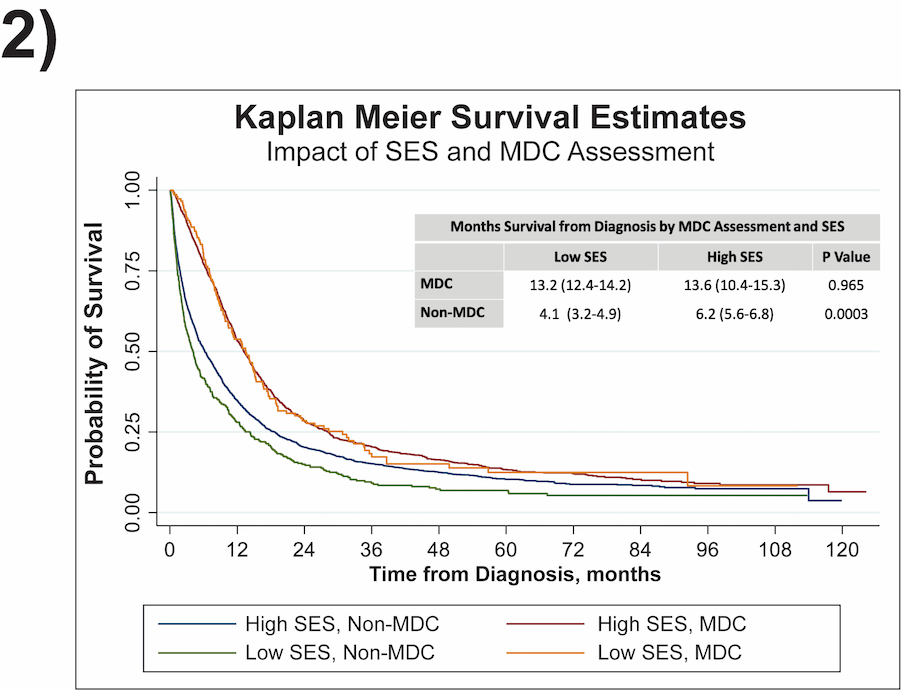
Survival from diagnosis (months) by multidisciplinary clinic (MDC) evaluation and socioeconomic status (SES).
Back to 2022 Abstracts
