COMPARATIVE OUTCOMES OF ANTI-REFLUX SURGERY IN OBESE AND MORBIDLY OBESE PATIENTS
Federico Palacardo, Jacques A. Greenberg*, Rodrigo C. Edelmuth, Caitlin Egan, Yeon Joo Lee, Felice Schnoll-Sussman, Philip O. Katz, Brendan M. Finnerty, Thomas J. Fahey, Rasa Zarnegar
Surgery, Weill Cornell Medicine, New York, NY
Introduction: Roux-en-Y gastric bypass has long been the preferred operation in the surgical management of obese patients with gastroesophageal reflux disease (GERD); however, some are hesitant to undergo bypass. Obese patients have a multifactorial predisposition to GERD, including lower esophageal sphincter (LES) dysfunction and aberrant pressure gradients across their diaphragmatic crura. Among non-obese patients, anti-reflux surgery (ARS) with hiatal hernia (HH) repair and LES augmentation has shown excellent long-term results. We aimed to determine whether patient satisfaction and GERD recurrence differed between patients with normal and elevated BMIs who underwent ARS.
Methods: Review of a prospectively-maintained database of consecutive patients that underwent elective robotic ARS between January 2012 and June 2021 was performed. Patients with previous foregut surgery, including ARS or bariatric operations, were excluded. Perioperative and postoperative characteristics were compared across three groups dependent upon BMI: normal (BMI?30), obese (30<BMI?35) and morbidly obese (BMI>35). Kruskal-Wallis tests and Chi-Square tests were used to compare continuous and categorical variables where applicable, respectively.
Results: Four-hundred thirteen patients were identified, of which 294 (71.1%) had normal BMI, 87 (21.1%) were obese and 32 (7.8%) were morbidly obese. Preoperative symptomatology was similar across groups, including DeMeester scores (30.8 IQR [17.8-45.7] vs. 33.8 IQR [22.5-52.6] vs. 27.5 IQR [16-48.9], p=0.38). Despite this, morbidly obese patients had higher preoperative manometric and EndoFLIP™ intra-balloon pressure at the LES than those with lower BMIs (manometric 16.4 IQR [8.9-27.1] vs. 14.6 IQR [6.5-21.4] vs. 27.9 IQR [13-35] mmHg, p=0.01; EndoFlip™ 22.0 IQR [17.5-27.9], vs. 27.1 IQR [17.9-32.4] vs. 26.9 IQR [20.9-31.7] mmHg, p=0.04). No difference in preoperative distensibility index was found. Post-operative GERD HRQL cumulative scores were surprisingly lower in the elevated BMI groups (8.46 SD (9.29) vs. 5.42 SD (7.79) vs. 3.63 SD (6.05), p=0.03) but overall satisfaction was similar (53.3% vs. 73.1% vs. 75% p=0.37) at a median of 25-months after ARS. Comparable rates of postoperative reflux (15.1% vs. 22.2% vs. 10.5%, p=0.40) and hiatal hernia recurrence (16.8% vs. 24.4% vs. 10.5%, p=0.33) were identified on postoperative barium swallow, as were rates of reoperation (6.1% vs. 6.9% vs. 6.3%, p=0.97).
Conclusions: Despite higher manometric and EndoFLIP™ LES pressures prior to ARS, obese and morbidly obese patients experienced comparable pre-operative GERD symptomatology to those with normal BMI. Post-operative satisfaction and radiographic outcomes were also similar between groups. ARS with HH repair and LES augmentation may therefore be appropriate for select patients across a range of BMIs, including in the morbidly obese.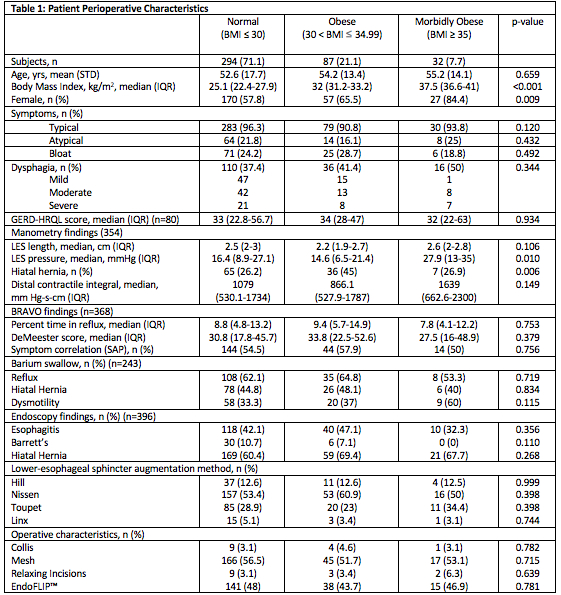
Continuous variables were compared using Kruskal Wallis test
Categorical variables were compared using Chi squared test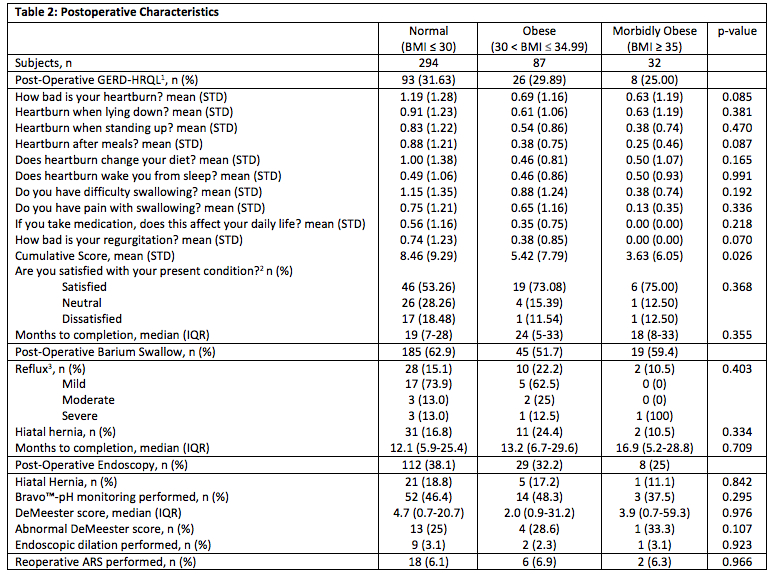
1Gastroesophageal Reflux Disease-Health Related Quality of Life
0: No symptoms
1: Symptoms noticeable but not bothersome
2: Symptoms noticeable and bothersome but not everyday
3: Symptoms bothersome every day
4: Symptoms affect daily life
5: Symptoms incapacitating to daily activities
2 Six patients did not complete response
3 Reflux grades variably reported
Continuous variables were compared using Kruskal Wallis test
Categorical variables were compared using Chi squared test
Back to 2022 Abstracts
