ROLE OF TUMORAL AND PERITUMORAL IMMUNE MICROENVIRONMENT IN PANCREATIC DUCTAL ADENOCARCINOMA: A POTENTIAL PREDICTOR OF PROGNOSIS
Ottavia De Simoni*1, Marco Scarpa2, Luca Dal Santo2, Antonio Scapinello1, Alberto Fantin1, Pierluigi Pilati1, Giada Munari1, Ylenia Spolverato2, Francesca Tolin1, Mario Gruppo1, Matteo Fassan2,1
1Istituto Oncologico Veneto Istituto di Ricovero e Cura a Carattere Scientifico, Padova, Veneto, Italy; 2Universita degli Studi di Padova, Padova, Veneto, Italy
Background
Pancreatic ductal adenocarcinoma (PDAC) is considered a highly immunosuppressive and heterogeneous neoplasm, characterized by a highly immunosuppressive tumor microenvironment (TME) and evasion of immune surveillance. TME plays a central role in modulating host immune response against cancer and, consequently, the prognosis. Determination of immune markers could be helpful in the management of patients. The aim of this study was to determine potential significant immune markers of prognosis, in order to consider them in surgical and oncological strategy.
Patients and methods
We retrospectively included patients with diagnosis of Resectable PDAC undergone surgery first with curative intent. Information on patient and clinical characteristics were collected through medical and pathological records. Immunohistochemical (IHC) staining using tissue microarray for PD-L1, CD3, CD4, CD8, FOXP3, CD20, INOS and CD163 was performed in order to characterize TME. Primary endpoint was Overall Survival (OS). For each immune marker, we calculated the threshold value (Youden's Index) of every ROC curve constructed on OS-1 year and OS-2 years. Based on these values, we performed survival analyses for dichotomized levels (low and high expression) of each immune marker.
Results
A total of 38 patients with diagnosis of PDAC undergone curative surgery were retrospectively analyzed. Pancreaticoduodenectomy was performed in 31(77%) patients, distal pancreatectomy in 7(17%). Median OS was 17 months (range 9-66). OS 1-year was 60%, OS 2-years was 36%. Lower density of CD3 intra-epithelial and FOXP3 intra- and peri-tumoral were associated with a trend to significance to better OS (AUC=0,78, p=0,051 and AUC=0,68, p=0,058). As shown in Figure 1, lower density of CD3 intra-epithelial and FOXP3 intra- and peri-tumoral are good predictor of long term survival (p=0.03 and p=0.04, respectively). Lower density of PD-L1 is a good predictor of long-term survival (p=.0004). ROC curve analyses revealed that lower infiltration of TAMs INOS+ intra- and peri-tumoral was significantly associated with long term survival (AUC 0,89, p=0,006). As shown in Figure 2, lower density of TAMs INOS+ and CD163 are good predictor of long-term survival (p=0.04 and p=0.03, respectively).
Conclusions
Despite the retrospective nature and small sample size, our study showed that lower infiltration of CD3+, FOXP3, PD-L1, TAMs INOS+ and CD163 are significant predictors of good prognosis. Preoperative possibility to analyze these potential immune markers could be useful and determinant in the staging process and in the decision making of the PDAC management.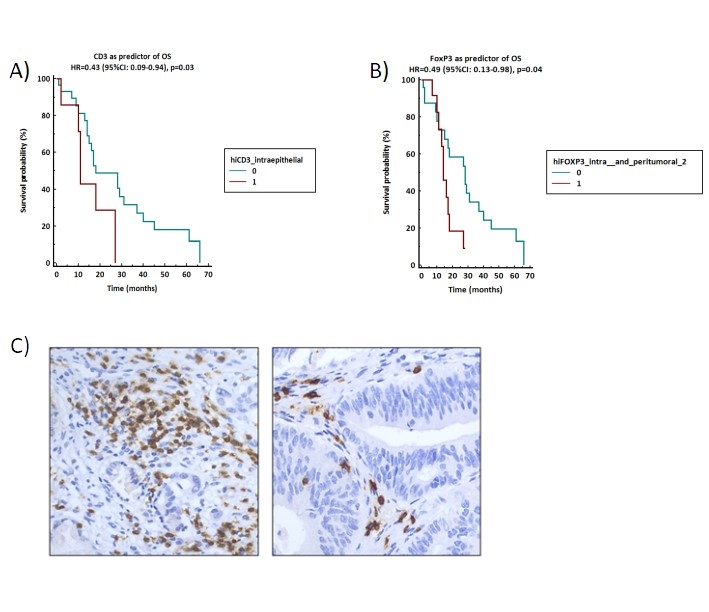
Figure 1. A-B) Survival analyses based on dichotomized density of CD3+ intra epithelial and FOXP3, respectively C) Representative example of high and low density expression of TILs CD3+ intra-epithelial in PDAC.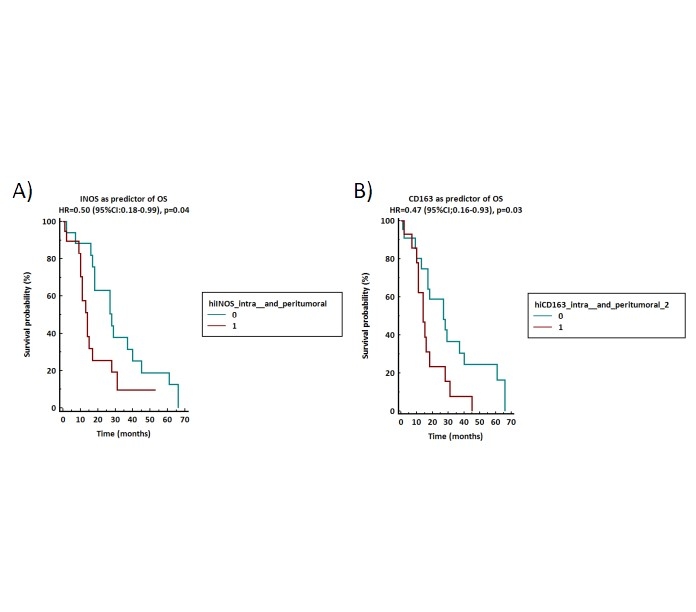
Figure 2. A-B) Survival analyses based on dichotomized density of TAMS INOS+ and CD163+.
Back to 2022 Abstracts
