THE IMPACT OF PERIOPERATIVE CHEMOTHERAPY ON CONDITIONAL SURVIVAL OF PATIENTS WITH LOCALLY ADVANCED RECTAL CANCER: SOMETHING IS BETTER THAN NOTHING.
Mohammed O. Suraju*1, Paolo Goffredo2, Sarah Bell1, Apoorve Nayyar1, Jeremy Chang1, Catherine Tran1, Dakota T. Thompson1, Imran Hassan1
1The University of Iowa Hospitals and Clinics, Iowa City, IA; 2Memorial Sloan Kettering Cancer Center, New York, NY
INTRODUCTION: Conditional survival (CS) is the probability of surviving additional years, after a given time interval from curative treatment. Metastatic disease is the primary cause for mortality after curative treatment for locally advanced rectal cancer (LARC) and systemic chemotherapy represents the main modality in decreasing this risk. Per guidelines, both neoadjuvant single-agent chemoradiation with multi-agent adjuvant chemotherapy (nCRT) and total neoadjuvant chemoradiation (TNT) are acceptable regimens. However, compliance with adjuvant chemotherapy is generally suboptimal, and a significant proportion of patients receive either none or tolerate only monoagent adjuvant therapy. Nonetheless, the prognostic implications of non-adherence to adjuvant regimens on CS have not been described. Moreover, achieving pathologic complete response (pCR) has been associated with favorable biology and improved overall survival (OS), but there is a scarcity of data on its impact on CS. We hypothesized that being alive at 3 years and having pCR would be a proxy for less aggressive biologic behavior and those patients would have higher rates of CS regardless of adjuvant regimens.
METHODS: The National Cancer Database (2010-2017) was queried for adult patients with stage II-III rectal cancer who underwent proctectomy with negative margins and received neoadjuvant chemoradiation. CS was investigated at 3 years.
RESULTS: A total of 18,067 patients survived at least 3 years after the diagnosis. The majority were Caucasian, had no comorbidities, and were <70 years; 43% had stage II disease, while 57% had stage III disease. Of those, 29% received complete nCRT, 16% received TNT, 14% received adjuvant monoagent chemotherapy, and 42% did not receive adjuvant therapy. The 5-year OS for the initial cohort was 86%, 82%, 84%, and 77%, respectively, while among those alive at 3 years, CS was 92%, 90%, 91%, and 89% (Figure 1). Rates of sphincter preserving surgeries did not differ among the groups. After adjustment for available confounders, no pCR and not receiving any adjuvant treatment were associated with both worse OS and CS (all p<0.01).
CONCLUSIONS: In this national cohort, we confirmed low rates of compliance to adjuvant chemotherapy regimens after neoadjuvant chemoradiation and proctectomy with 14% of patients receiving incomplete and 42% no adjuvant treatment. Compared to multiagent regimens, not receiving adjuvant therapy was associated with lower OS and CS, while monoagent was not. These findings were independent from having pCR, which was a positive prognostic factor for both OS and CS. Therefore, these data support administration of adjuvant treatment even among those patients with favorable biology, although a subset of LARC patients might be candidates for de-escalation of adjuvant chemotherapy in the form of monoagent therapy alone.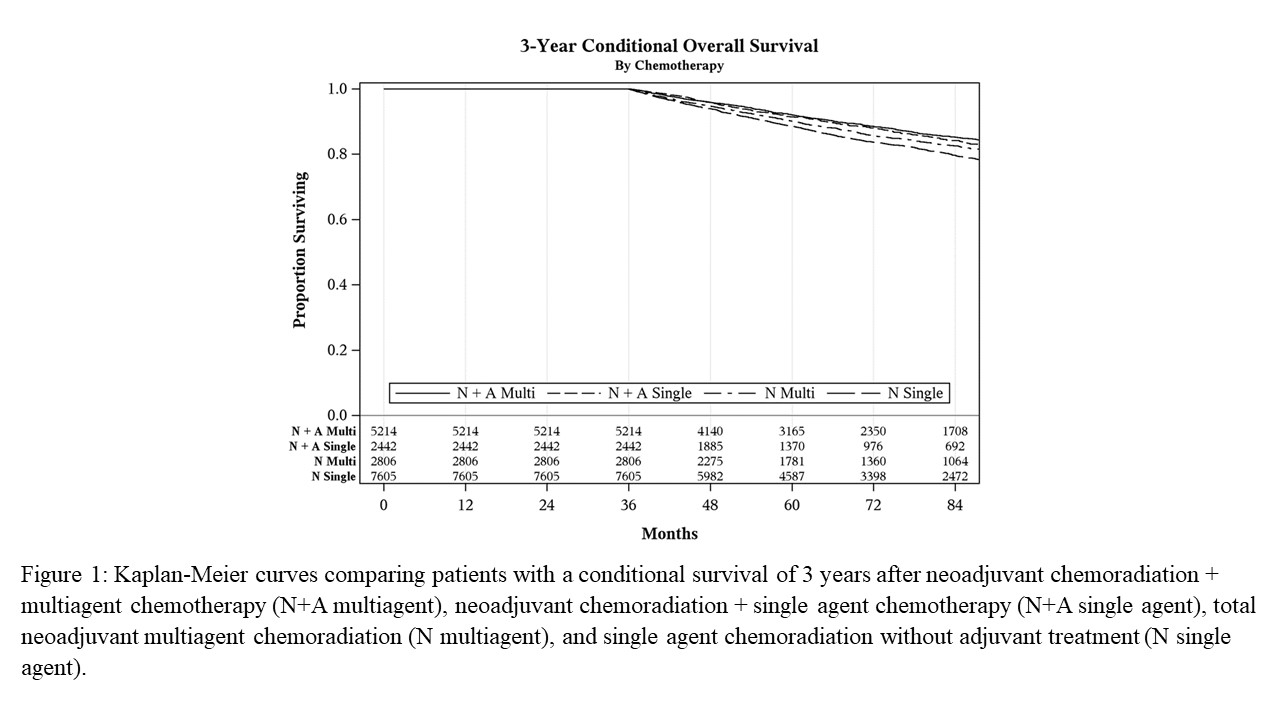
Back to 2022 Abstracts
