INTENSIVE CARE UNIT OBSERVATION AFTER PANCREATECTOMY: TREATING THE PATIENT OR THE SURGEON?
Thomas L. Sutton*, Kristin C. Potter, Jack P. O'Grady, Michael Aziz, Skye C. Mayo, Rodney Pommier, Erin W. Gilbert, Flavio G. Rocha, Brett C. Sheppard
Surgery, Oregon Health and Science University, Portland, OR
Introduction:
Routine intensive care unit admission (ICUA) is commonplace following pancreatectomy, particularly pancreaticoduodenectomy, and aims to allow early postoperative complications to occur in a high acuity setting. The value of this practice in avoiding failure-to-rescue or impacting perioperative mortality is poorly studied, however.
Methods:
We queried our institutional National Surgical Quality Improvement Project (NSQIP) database for patients undergoing pancreatectomy from 2013-2020. Initial postoperative dispositions, ICU courses, subsequent ICU transfers, and hospital cost data in United States Dollars (USD) were reviewed. Patients were analyzed in three groups by postoperative disposition and level of care as defined by the Society of Critical Care Medicine: those with ICUA requiring ICU-level care (e.g., invasive ventilation, vasopressors, inotropes, intravenous antiarrhythmics), those with ICUA requiring ward-level care, and those admitted to the ward. Data were analyzed with multivariable logistic regression.
Results:
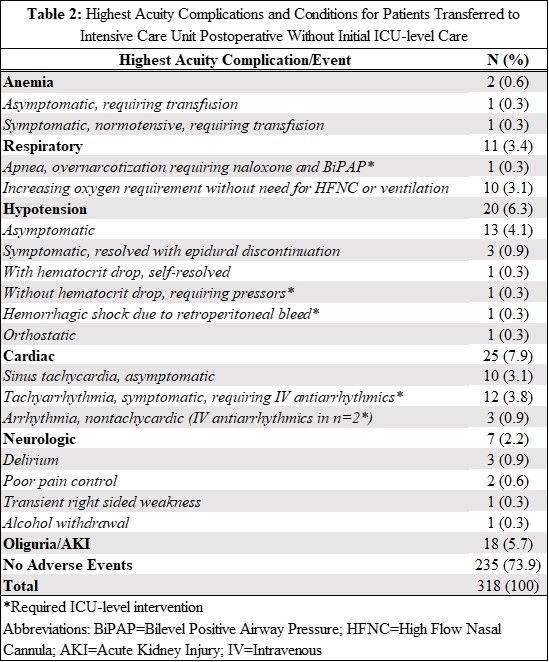
Six-hundred-thirty-seven patients were identified; 404 (63%) underwent pancreaticoduodenectomy (Table 1). At postoperative admission, two-thirds (n=318, 63%) of patients were only receiving ward-level interventions. Of 318 patients with ICUA requiring ward-level care, 235 (74%) had no identified disturbances or complications, 66 (21%) had minor disturbances requiring ward-level care, and 17 (5%) required ICU-level interventions during initial ICUA, most commonly antiarrhythmic infusion (n=12, Table 2). 30-day and 90-day mortality in patients requiring ICU-level interventions was 5% (n=10) and 8% (n=16) versus 0.3% (n=1) and 1.2% (n=4) in those without, respectively. Hospital length of stay was significantly longer with initial ICU-level interventions (median 11 versus 9 days, P<0.001), as were total ICU costs (mean 8683 versus 14611 USD, P<0.001).
On multivariable analysis, factors associated with higher odds of requiring ICU-level care at case closure were older age (OR 1.04/year, P<0.001), additional NSQIP-defined comorbidities (OR 1.34/comorbidity, P=0.003), pancreaticoduodenectomy (OR 1.93, P=0.04), higher intraoperative blood loss (OR 3.88/liter, P<0.001), longer surgical duration (OR 1.44/hour, P<0.001), and higher intraoperative crystalloid volume (OR 1.11/liter, P=0.008. There were no identified factors associated with new ICU-level interventions in patients admitted to ICU for observation.
Conclusion:
At high-volume pancreas centers, patients undergoing pancreatectomy who require only ward-level care at ICUA are at very low risk of requiring ICU-level care during observation, or of 30- and 90-day mortality. In patients with ward-level care needs postoperatively, ward admission with a low threshold for care escalation presents a significant opportunity for costs-savings and un-burdening ICUs.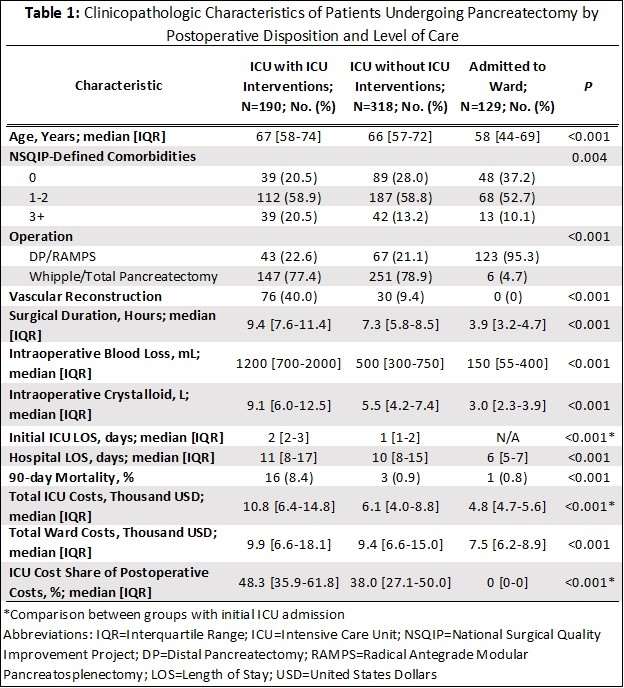
Back to 2022 Abstracts
