EXPLORING INTERACTIONS INVOLVING THE VOLUME-OUTCOME ASSOCIATION IN PATIENTS UNDERGOING PANCREATECTOMY FOR PANCREATIC ADENOCARCINOMA
Holly Spitzer*1, Panfeng Liang2, Samuel Grasso1, Elizabeth L. Carpenter3, Timothy J. Vreeland3, Amy Wagler2, Daniel Nelson1
1Department of Surgery, William Beaumont Army Medical Center, El Paso, TX; 2Department of Mathematical Sciences, The University of Texas at El Paso, El Paso, TX; 3Department of Surgery, Brooke Army Medical Center, San Antonio, TX
Background: Evidence has accumulated establishing a link correlating high facility operative case volume and improved outcomes for patients undergoing high-risk operations. Less is understood regarding the factors that may be moderating the volume-outcome association. Patient-level disparities associated with access to care are at least one hypothesis that has been proposed to explain these differences. We sought to examine the volume-outcome relationship among matched patients undergoing pancreatectomy for pancreatic adenocarcinoma and explore interactions within the models to identify factors that may explain observed outcome variance.
Methods: The 2004-2011 Nationwide Inpatient Sample was queried for patients undergoing pancreatectomy for pancreatic adenocarcinoma. Hospitals were stratified by annual case volume and baseline patient and hospital characteristic were compared. Propensity score matching (PSM) was performed. Primary outcomes included length of stay (LOS), composite inpatient morbidity and inpatient mortality.
Results: Among 5,692 patients identified 19.7% underwent surgery at a high-volume center (HVC), while the majority were treated at medium-volume centers (61.5%). Prior to PSM, compared to HVC, low-volume centers (LVC) more frequently treated uninsured and those with government aid, patients of minority race and those with higher Elixhauser Index (EI) comorbidity scores (all p<0.05). LOS (6 vs 9 days; p<0.001), composite inpatient morbidity (6.9% vs 11%; p=0.01) and inpatient mortality (2.1% vs 6.8%; p<0.001) were better at HVC compared to LVC. After PSM, differences in payer status, race and comorbidity scores were eliminated. In this adjusted population, LOS (8.2 vs 10.2 days; p<0.001) and inpatient mortality (2.1% vs 4.6%; p=0.02) remained better at HVC compared to LVC, however, composite inpatient morbidity was no longer different (6.9% vs 7.8%; p=0.8). Global model comparison (GMC) tests, using survey-weighted Satterthwaite adjustments, applied to matched-data models for the primary outcomes indicated no significant interactions between covariates for LOS or morbidity models. However, the GMC test provides evidence of significant interaction between EI and volume on mortality (P<0.001), indicating that the volume effect on mortality is moderated by patient EI score. Specifically, as EI score increases, mortality improves at HVC compared to LVC (Figure).
Conclusion: Ethical regionalization of high-risk operations requires understanding complex interactions that may be driving the benefits associated with hospital operative volume. From a healthcare utilization standpoint, this data suggests that selective referral of high-risk patients to high-volume centers is warranted, as these are the patients most likely to benefit.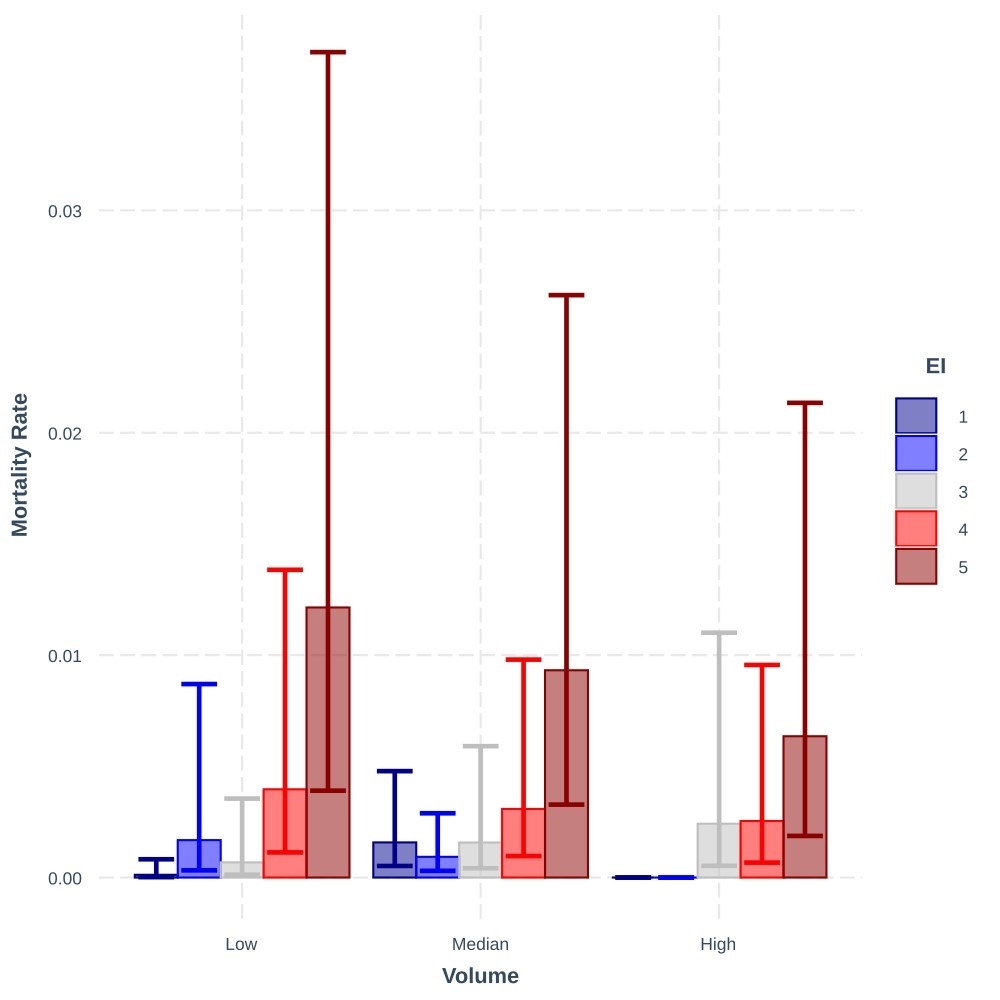
Relationship Between EI Score and Mortality Stratified by Hospital Operative Volume Among Patients Undergoing Pancreatectomy for Pancreatic Adenocarcinoma
Back to 2022 Abstracts
