OPIOID REDUCTION FOLLOWING MINIMALLY INVASIVE LIVER SURGERY: AIMING BEYOND INCISION SIZE
Russell G. Witt*, Raymond Traweek, Elsa M. Arvide, Sa Nguyen, Naruhiko Ikoma, Timothy E. Newhook, Ching-Wei D. Tzeng, Yun Shin Chun, Jean-Nicolas Vauthey, Hop Tran Cao
Surgery, The University of Texas MD Anderson Cancer Center Division of Surgery, Houston, TX
Background: Opioid abuse and dissemination continues to be a significant public health problem with a record number of drug overdose deaths in 2020. While minimally invasive surgeries are believed to reduce opioid use compared to open surgery, the impact of educational initiatives and prescribing guidelines is less clear. We assessed changes in prescribing practices following an opioid education and prescribing initiative for patients undergoing minimally invasive liver surgery.
Methods: Using a prospectively maintained single-institutional database of all patients undergoing minimally invasive liver surgery, clinical characteristics, non-opioid adjunct utilization, and inpatient oral morphine equivalents (OME, intraoperative, inpatient, and discharge prescriptions) were compared between patients treated before (1/2017-7/2018) and after (8/2018-11/2021) implementation of a departmental opioid education and prescribing guideline initiative. Pain scores were measured for the duration of their admission.
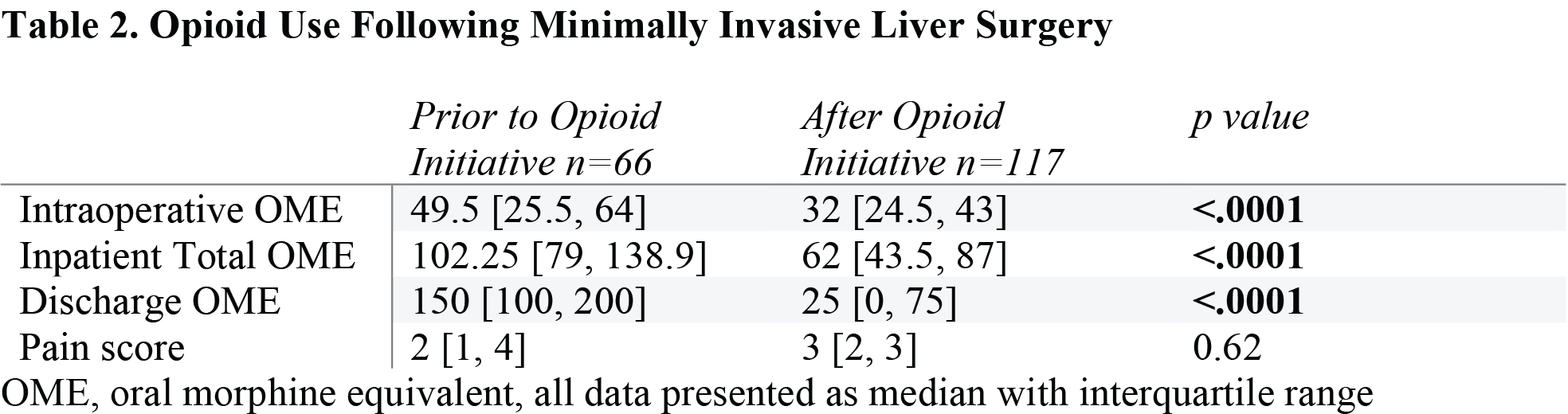
Results: Of 183 total patients, 66 underwent surgery before and 117 after opioid reduction initiatives. There were no significant differences between groups with respect to baseline clinical characteristics including patient demographics and disease type (Table 1). Operative approaches shifted over the course of the study with increased utilization of robotic surgery and decreased utilization of both laparoscopic and hand-assisted liver surgery (p<.0001). Length of stay and operative complexity were similar between the two cohorts. Regional anesthetic block rates increased after implementation of opioid reduction initiatives (18 (31%) before, 103 (88.8%) after). Intraoperative, inpatient, and discharge OME were significantly fewer (Table 2, p<.0001) after the opioid intervention, with median discharge OME decreasing from 150mg to 25mg.
Conclusions: Intentional efforts to curb opioid overpresciption through implementation of an education initiative and prescribing guidelines successfully reduced both intraoperative and discharge OME in minimally invasive liver surgery, without increasing pain scores. Mindful stewardship of opioid use is applicable even with minimally invasive surgery.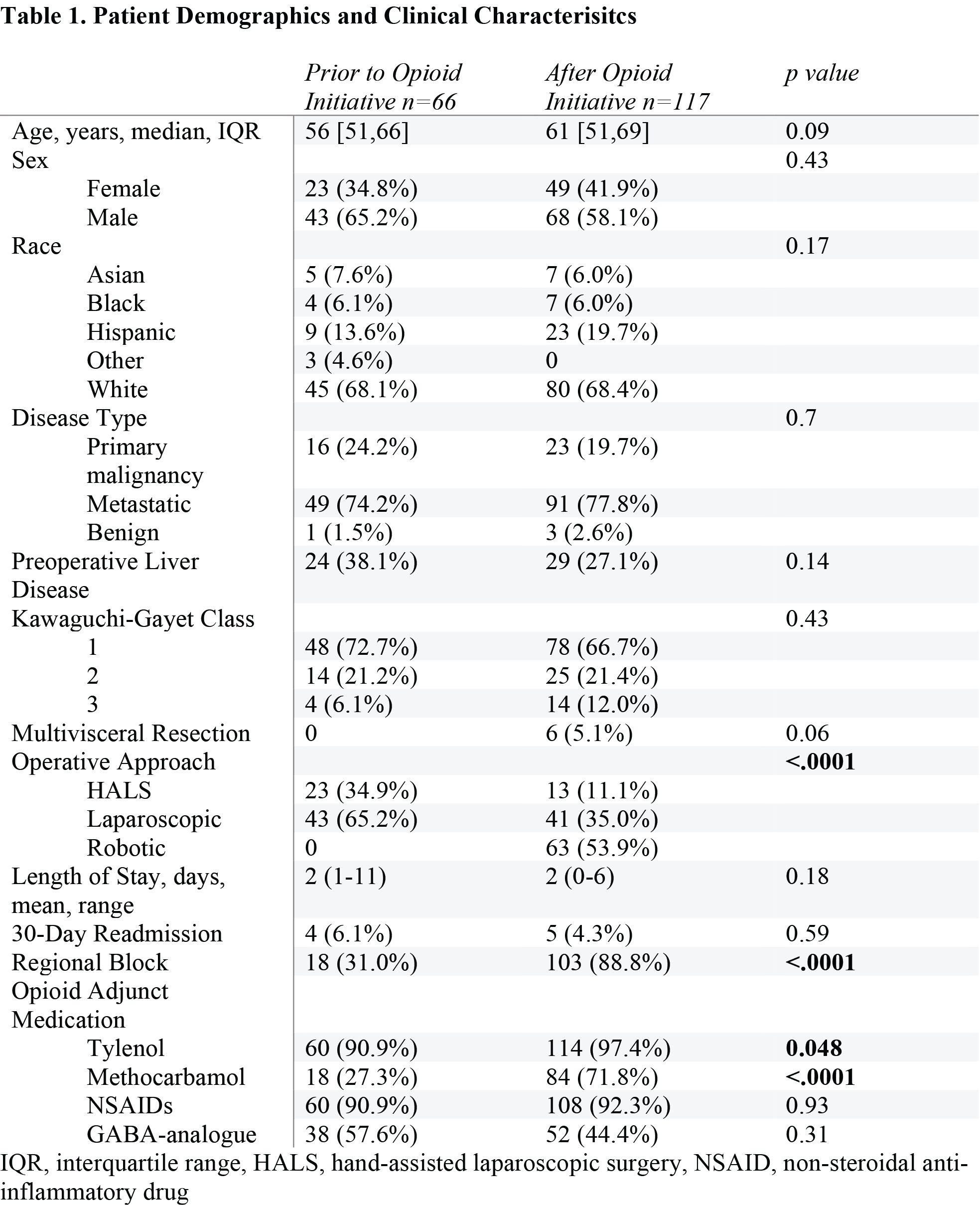
Back to 2022 Abstracts
