COMPARISON OF SURGICAL OUTCOMES FOLLOWING PANCREATIC SURGERY BETWEEN THE VETERAN AFFAIRS HEALTH SYSTEM (VHA) AND NSQIP PARTICIPATING INSTITUTIONS
Lucas Keller-Biehl*1,2, Alexander Simmonds1,2, Wayne Tse1,2, Adam Khader1,2, Leopoldo Fernandez1,2, Michael Amendola1,2
1Surgery, Virginia Commonwealth University, Richmond, VA; 2VA Richmond Medical Center, Richmond, VA
Introduction: Previous studies have indicated differing outcomes following pancreatic resection (PR) surgery in the VHA compared to other non-governmental health systems. VHA surgical outcomes are followed by the Veteran Affairs Surgical Quality Improvement Program (VASQIP) and outside the VHA by participating National Surgery Quality Improvement Project (NSQIP) systems. We set forth to examine PR outcomes as captured in VASQIP and NSQIP.
Methods: VASQIP and NSQIP were examined with CPT Codes (48140, 48145, 48146, 48148, 48150, 48152, 48153, 48154) for all PR reported from 2015 to 2019. Patient demographics, comorbidities, and postoperative outcomes were compared. Pearson's ?2*, binary logistic regression**, and students t *** (SPSS 27.0) were used to analyze differences.
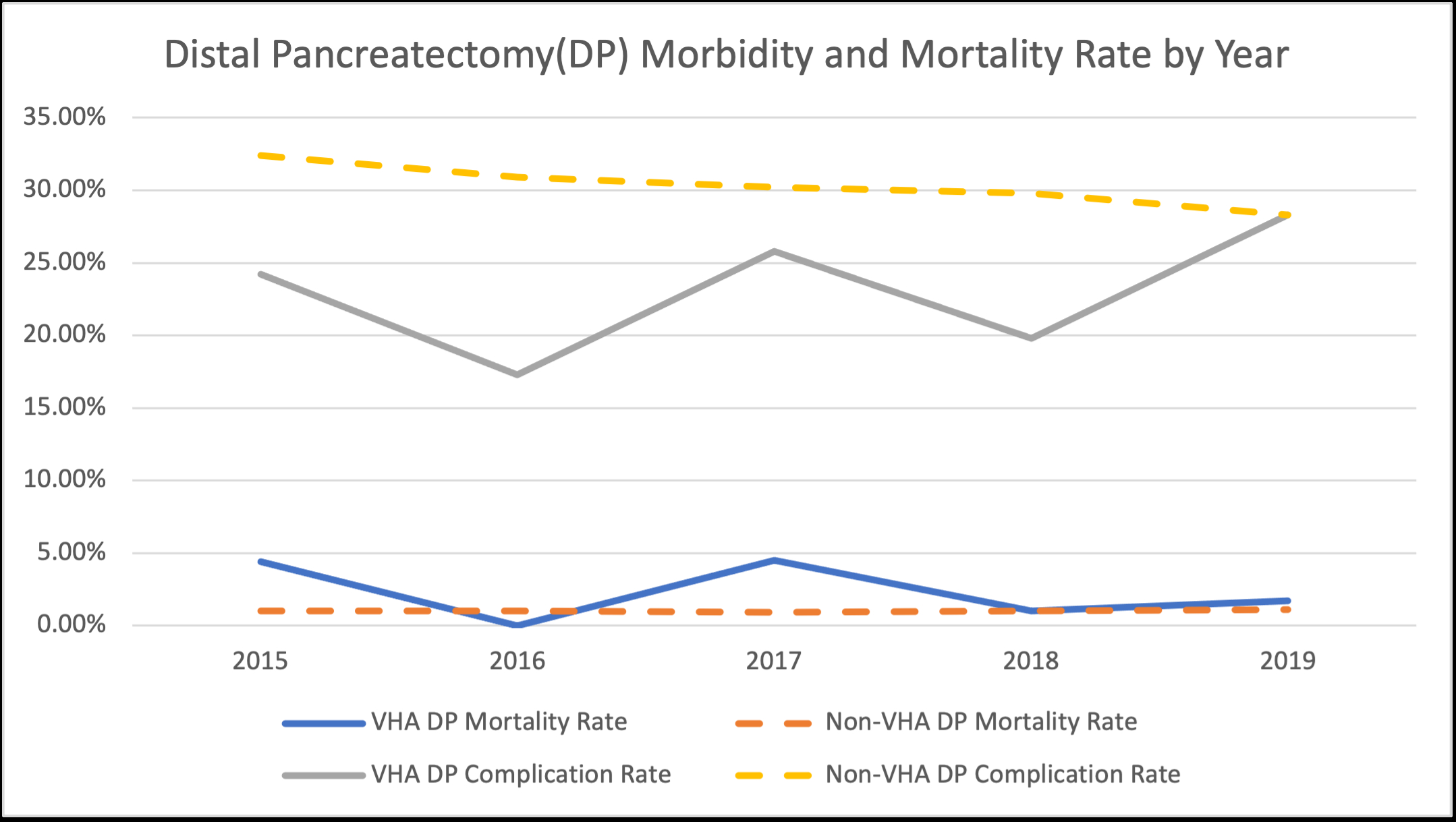
Results: A total of 1,198 PR were reported in the VASQIP and 39,834 in NSQIP over the period examined. VHA patients were 94.5% male with the majority white (70.8%) compared to 50.8% male and 73.3% white within the NSQIP cohort. VHA patients were older (66.2 +/- 8.9 vs 63.8 +/- 12.6, p<0.001***) and had more comorbidities compared to non-VHA patients (2.1 +/- 1.3 vs 1.1 +/- 0.9, p<0.001***). VHA patients had a lower complication rate following whipple (36.8% vs 45.1%, p<0.001* OR 0.7 95% CI 0.6-0.8) or distal pancreatectomy (DP) (22.4% vs 30.3%, p<0.001* OR 0.7 95% CI 0.5-0.8), however, a higher 30-day mortality rate for both whipple (3.5% vs 2.2%, p=0.014*, OR 1.7 95% CI 1.1-2.4) and DP (2.2% vs 1.0%, p=0.014*, OR 2.2 95% CI 1.2-4.4). A binary logistic regression revealed factors that predicted post-operative mortality were male sex (p<0.001** OR 1.4 95% CI 1.1-1.6), cardiac history (p<0.001** OR 2.2 95% CI 1.4-3.5), disseminated cancer (p=0.044** OR 1.4 95% CI 1.0-1.9), dialysis (p<0.001** OR 7.4 95% CI 4.0-13.7), hypertension (p=0.003** OR 1.4 95% CI 1.2-1.7), ascites (p<0.001** OR 4.5 95% CI 2.1-9.5), COPD (p<0.001** OR 1.7 95% CI 1.3-2.3), and age (p<0.001** OR 1.05 95% CI 1.04-1.06). Mortality following DP coincided with male sex (p=0.001** OR 1.8 95% CI 1.3-2.5), cardiac history (p=0.003** OR 3.1 95% CI 1.5-6.5), disseminated cancer (p<0.001** OR 2.3 95% CI 1.4-3.6), dialysis (p<0.001** OR 7.6 95% CI 3.2-17.9), and age (p<0.001** OR 1.05 95% CI 1.03-1.06). Being a VHA patient was not significant in predicting postoperative mortality in the multivariate analysis.
Conclusion: PR resections in and outside the VHA Systems had similar mortality and morbidity rates despite the VHA having older patients with more comorbidities. Importantly, being a VHA patients was not an independent predictor of worse outcomes following PR.
Limitation: The use of two separate databases with potentially different reporting requirements likely explains differing complication rates.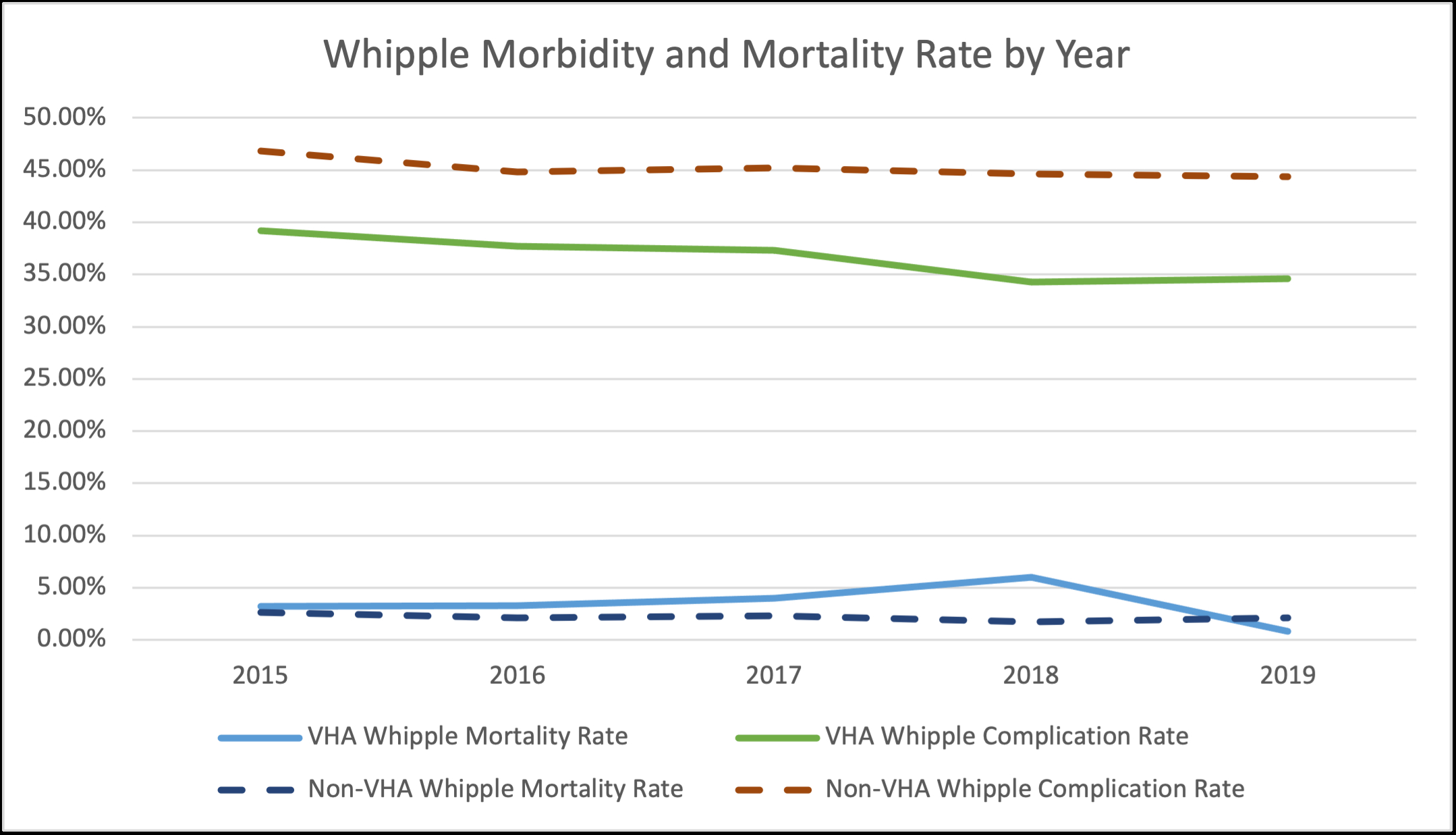
Back to 2022 Abstracts
